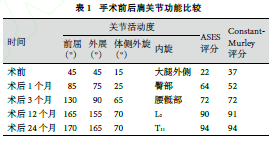
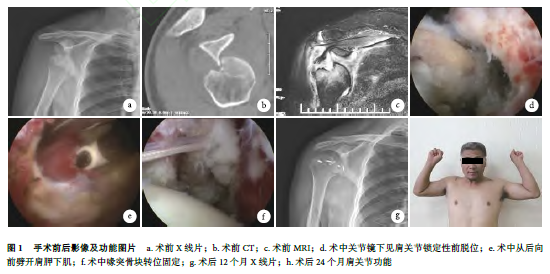
关节镜下改良弹性固定Latarjet术治疗一例慢性锁定性肩关节前脱位
2019-01-28 黄刚 中国修复重建外科杂志
慢性锁定性肩关节前脱位是指肩关节前脱位3周后未复位或无法复位者,可能导致肩部肌肉进行性萎缩和肩部活动范围受限,以及继发严重血管和神经损伤。由于锁定的脱位关节与周围组织粘连严重,复位困难,通常采用切开复位或关节置换治疗,目前未见采用全关节镜下治疗成功的病例报道。2016年7月,我们采用关节镜下改良弹性固定Latarjet术治疗1例慢性锁定性肩关节前脱位患者,获得满意效果。报告如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前脱位#
53
#锁定性#
40
#肩关节#
47
#关节镜#
42
#ATA#
30
#脱位#
0
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
64