2022年3月25日,诺华(中国)双靶向联合治疗药物泰菲乐®(甲磺酸达拉非尼胶囊)和迈吉宁®(曲美替尼片),于日前获国家药品监督管理局批准新增适应症,用于治疗BRAF V600突变阳性转移性非小细胞肺癌。这不仅是泰菲乐®联合迈吉宁®获批的第三个适应症,也是目前中国首个批准针对BRAF V600突变阳性转移性非小细胞肺癌的双靶向联合治疗药物。
此前,泰菲乐®和迈吉宁®已获批用于治疗BRAF V600突变阳性的不可切除或转移性黑色素瘤及BRAF V600突变阳性的Ⅲ期黑色素瘤患者完全切除后的辅助治疗。这也就意味着中国肺癌少见突变的患者带来新的治疗选择,是肺癌靶向治疗领域又一重要的里程碑。
诺华肿瘤(中国)总经理方爱莎(Isabel Afonso)女士表示:“诺华始终将患者的健康置于首位。为满足多样化的临床需求,诺华持续将多款肺癌治疗药物陆续引入中国,为包括少见靶点在内的众多肺癌患者带来更为丰富的创新疗法及解决方案,与中国医生一道,为患者缔造健康福祉。”
BRAF V600突变,患者临床获益有限
肺癌是中国发病率和死亡率均排在第一位的恶性肿瘤,其中非小细胞肺癌(NSCLC)约占肺癌的85%。在NSCLC中,BRAF 基因突变率为1.5%-3.5%;BRAF V600约占所有BRAF突变的50%,其中最常见类型为V600E突变。国内外研 究显示,NSCLC中的BRAF突变在男女比例和吸烟状态等方面的差异并不一致,而在病理学类型上,BRAF突变(尤其 是BRAF V600E突变)的NSCLC患者均以腺癌为主。
BRAF驱动基因是丝裂原活化蛋白激酶(MAPK)通路的关键分子,BRAF突变可导致MAPK下游细胞信号转导通路的持续激活,促使细胞生长、增殖,介导肿瘤发生。根据对RAS激酶的依赖性和RAF的二聚化特征,BRAF突变可分为Ⅰ、Ⅱ、Ⅲ类。 其中,Ⅰ类突变为RAS激酶非依赖性,具有高激酶活性单体,以BRAF V600突变为代表;Ⅱ类突变为RAS激酶非依赖性,具有激酶活性的二聚体,如G464和G469突变;Ⅲ类突变为RAS激酶依赖性,无激酶活性的异源二聚体,包括D594和 G466突变。中国研究显示,在BRAF 突变NSCLC患者中,Ⅰ、Ⅱ和Ⅲ类BRAF突变比例分别为32%、21%和13%。
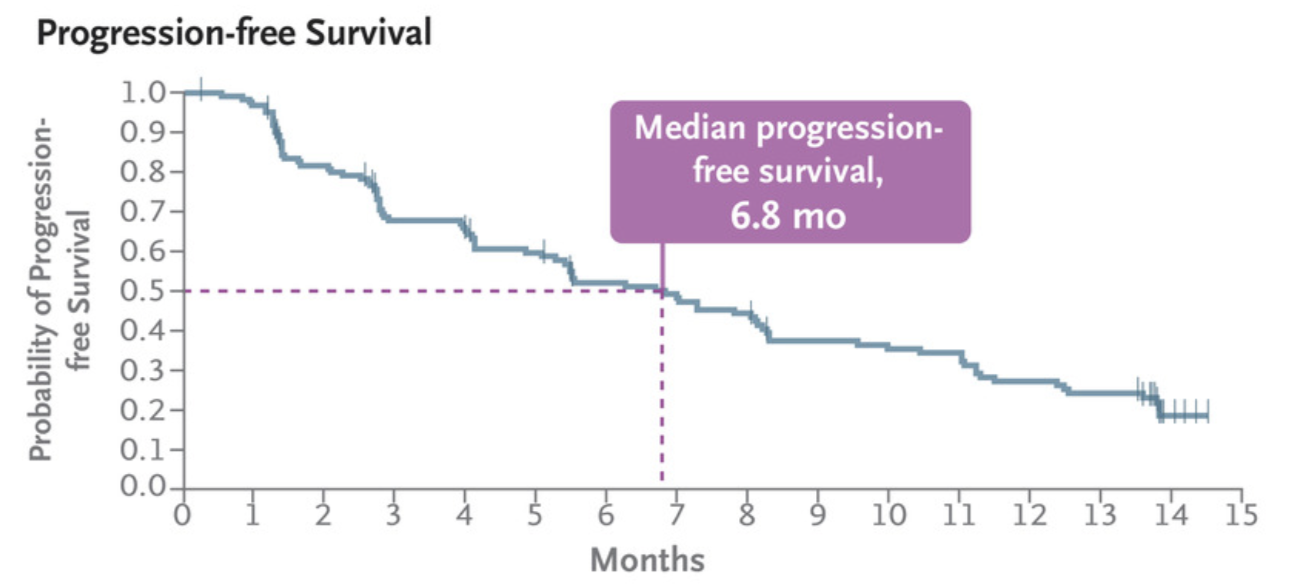
目前,针对BRAF V600突变患者的化疗和免疫治疗的临床获益并不理想,预后差,总生存期较短。研究显示,化疗的无进展生存期(PFS)仅为1.5~4.2个月,免疫检查点抑制剂治疗BRAF突变NSCLC患者的PFS也只有2.5~5.3个月。而近年来随着“精准医疗”的兴起,肺癌分子靶向药物逐渐成为主要治疗手段之一,为肺癌BRAF突变患者带来了新的希望。
破解BRAF V600突变,开启NSCLC靶向治疗新里程
在BRAF V600E突变NSCLC患者中,小分子靶向药展现出了良好的治疗前景。临床研究表明,BRAF抑制剂达拉非尼联合MEK抑制剂曲美替尼的治疗方案能够显著延长此类患者的生存期,且安全性可控。据悉,该方案已被NCCN、 ESMO和CSCO等国内外多个指南推荐作为BRAF V600E/V600突变NSCLC的一线治疗选择。
达拉非尼联合曲美替尼双靶组合采用全面抑制MAPK的上下游通路的创新机制。达拉非尼是一种选择性BRAF激酶活性抑制剂;曲美替尼是一种可逆的、高选择性MEK1和MEK2激酶活性的变构抑制剂,两者联合应用可以同时抑制BRAF和MEK两个靶点,使病灶得到快速且显著的缓解。
全球多中心、开放标签的Ⅱ期试验CDRB436E2201,分别证明达拉非尼作为单药治疗经治患者(队列A)、联合曲美替尼治疗经治患者(队列B)以及联合曲美替尼治疗初治患者(队列C)均具有显著疗效,客观缓解率(ORR)分别为33.0%、63.2%和64.0%,PFS分别为5.5、9.7和14.6个月。根据这个研究美国FDA批准了达拉非尼联合曲美替尼治疗BRAF突变肺癌的适应症。近期,该研究的5年长期生存随访数据还报告了经治和初治患者的5年OS率分别为19%和22%,作为BRAF V600E突变NSCLC第一个长期随访数据,进一步验证了达拉非尼联合曲美替尼对于BRAF V600突变的晚期NSCLC的疗效。真实世界研究GFPC 01-2019则在前瞻性临床试验基础上进一步证实,对于BRAF V600E突变的晚期NSCLC患者,达拉非尼联合曲美替尼是一种有效治疗方式。
本次中国适应症获批是基于达拉非尼联合曲美替尼治疗中国人群BRAF突变阳性转移性NSCLC的注册临床研究。该研究是由中山大学肿瘤防治中心张力教授牵头的全国多中心Ⅱ期临床试验,研究证实了达拉非尼联合曲美替尼对于BRAF V600E突变的转移性NSCLC具有优异的疗效,研究结果将于近期国际大会报道发布。
“达拉非尼联合曲美替尼治疗BRAF突变肺癌方案在国内获批是一件振奋人心的事情,使得BRAF V600成为继EGFR、ALK、ROS1之后,成为晚期NSCLC又一个可靶向基因突变,这是肺癌靶向治疗领域又一重要的里程碑。”中山大学肿瘤防治中心肿瘤内科主任、肺癌首席专家张力教授表示,“BRAF V600突变是晚期NSCLC的少见驱动基因,既往缺乏有效的治疗方案,患者预后较差。达拉非尼联合曲美替尼中国肺癌注册研究和全球CDRB436E2201系列研究表明,无论作为一线治疗还是后线治疗,达拉非尼联合曲美替尼治疗BRAF V600突变NSCLC患者均具有良好的疗效,对比单靶、化疗和免疫治疗,达拉非尼联合曲美替尼显示出疗效优势。同时,相较于全球CDRB436E2201研究,结合数据分析发现中国肺癌患者对于达拉非尼联合曲美替尼的有效性与全球一致。此前,达拉非尼联合曲美替尼在晚期黑色素瘤和黑色素瘤辅助治疗中已展现出显著的疗效,本次获批让我们对于BRAF突变肺癌又多了一种有效的治疗手段,也为靶向治疗在NSCLC患者辅助治疗开启了新的方向。此外,口服给药的方式也让患者更加便捷、依从性更高。”该方案已被美国国家综合癌症网络NCCN、欧洲肿瘤内科学会ESMO和中国临床肿瘤学会CSCO等国内外多个指南推荐作为BRAF V600E/V600突变NSCLC的一线治疗选择。
诺华全球药品开发(中国)负责人王兴利医学博士表示:“‘以患者为中心’贯穿于诺华整个研发环节。针对此次达拉非尼联合曲美替尼的新适应症,从研究设计开始,我们就在努力寻找合理且高效的路径,力求尽快把新药带给患者。未来,我们还将继续加速更多中国高发肿瘤新药的全球同步研发及上市。”
作为全球领先的跨国药企,诺华目前已经有多款肺癌治疗药物获批,在肿瘤领域更拥有覆盖乳腺癌、肺癌、黑色素瘤、肾癌以及血液疾病等广泛的产品组合和丰富的产品线。诺华致力于提升创新药品的可及性,让更多中国患者尽快获益于创新成果,为他们带来健康和希望。
参考资料
1, Planchard D, Smit EF, Groen HJM, et al. Dabrafenib plus trametinib in patients with previously untreated BRAFV600E-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 2017 Oct;18(10):1307-1316. doi: 10.1016/S1470-2045(17)30679-4.
2, Planchard D, Besse B, Groen HJM, et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol. 2016 Jul;17(7):984-993. doi: 10.1016/S1470-2045(16)30146-2.
3, Odogwu L, Mathieu L, Blumenthal G,et al. FDA Approval Summary: Dabrafenib and Trametinib for the Treatment of Metastatic Non-Small Cell Lung Cancers Harboring BRAF V600E Mutations. Oncologist. 2018 Jun;23(6):740-745. doi: 10.1634/theoncologist.2017-0642.
4, AULIAC J B, BAYLE S, DO P, et al. Efficacy of dabrafenib plus trametinib combination in patients with BRAF V600E-mutant NSCLC in real-world setting: GFPC 01-2019[J]. Cancers (Basel), 2020, 12(12): E3608.
5, AULIAC J B, BAYLE S, DO P, et al. Efficacy of dabrafenib plus trametinib combination in patients with BRAF V600E-mutant NSCLC in real-world setting: GFPC 01-2019[J]. Cancers (Basel), 2020, 12(12): E3608.
6, 中国临床肿瘤学会. 非小细胞肺癌诊疗指南 (2021)[M]. 北京: 人民卫生出版社, 2021.Chinese Society of Clinical Oncology. Guidelines for diagnosis and treatment of non-small cell lung cancer (version 2021) [M]. Beijing: People’s Medical Publishing House, 2021.
7,赵媛媛, 周建英, 范云, et al. BRAF V600突变型非小细胞肺癌的治疗进展[J]. 中国癌症杂志, 2021, 31(12):8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
63
#肺癌患者#
58
#突变型#
51
#适应症#
54
#BRAF#
53
#达拉非尼#
37
#新适应症#
43
#非小细胞肺癌患者#
54