JAMA Network Open:对于收缩压低于130mmHg的成人,更佳舒张压范围是多少?
2021-02-19 MedSci原创 MedSci原创
研究结果表明,舒张压低于60mmHg可能是有害的,而舒张压在70至80mmHg之间是收缩压低于130mmHg的患者的最佳目标。
高血压是心血管疾病和死亡最重要的可改变的危险因素之一。随着时间的推移,人们对BP的普遍看法发生了巨大变化。Framingham心脏研究的结果表明收缩压是心血管预后的一个更重要的危险因素,将重点从舒张压(DBP)转移到收缩压(SBP)。而对于DBP在心血管风险评估中的作用是否被忽视引发了一些争论。是否存在舒张J形现象,即高DBP和低DBP都可能增加心血管风险,是最有争议的问题之一。
关于舒张J形现象的争论起源于对低舒张压和心肌梗死死亡风险增加的观察。尽管有研究表明舒张压和心血管风险之间存在线性关系,更多的研究报道了舒张J形现象。但似乎可以肯定,极低的舒张压是有害的。2017年美国心脏协会(AHA)高血压指南建议强化血压目标值低于130/80 mmHg,但没有建议DBP的下限。而收缩压急剧降低可能会导致舒张压的过度降低,考虑到潜在的舒张J形现象,治疗的损害-益处方程将转向损害。为避免潜在危害,2018年欧洲心脏病学会(ESC)高血压指南建议所有风险水平患者的最佳舒张压目标为70至80 mmHg。
为了评估收缩压治疗后小于130 mmHg的患者是否存在舒张J形现象,并探讨该患者的安全最佳舒张压范围。研究者进行了相关的试验分析,将14094例患者随机分为强化血压控制(即收缩压和降压120 mmHg)和标准血压控制(即收缩压和降压140mm Hg)两组。以确定收缩压小于130 mmHg时舒张J形现象是否明显;其次,研究在指南推荐的收缩压小于130 mmHg时,安全和最佳舒张压范围。该研究结果近日发表在JAMA Network Open期刊上。

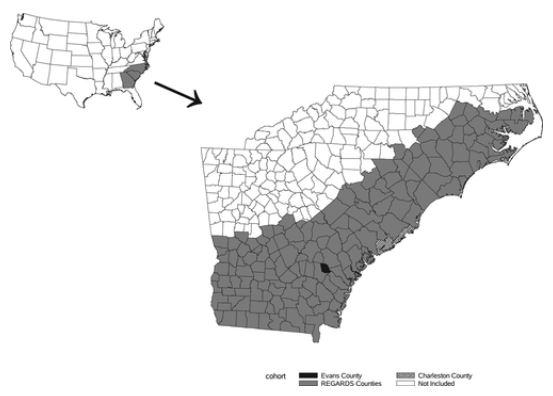
这项队列研究分析了心血管高危患者的结果数据,这些患者被随机分为强化血压控制组或标准血压控制组,在收缩压干预试验(SPRINT)中治疗后收缩压低于130mmHg,并采取措施控制糖尿病血压的心血管风险(ACCORD-BP)。数据收集时间为2010年10月至2015年8月(SPRINT)和1999年9月至2009年6月(ACCORD-BP)。数据分析从2020年1月到5月。
治疗后的舒张压,间隔为<60、60-70、70-80、80mmHg及以上。主要转归为全因死亡、非致死性心肌梗死和非致死性卒中的复合转归。综合心血管结果,包括心血管死亡、非致死性心肌梗死和非致死性卒中,是关键的次要结果。
研究结果显示,共有7515名患者(平均[SD]年龄65.6[8.7]岁;4553[60.6%]男性)被纳入该分析。舒张压在70-80mmHg之间时,主要转归、复合心血管转归、非致命性心肌梗死和心血管死亡的风险最低。平均舒张压低于60mmHg与主要转归(危险比[HR],1.46;95%CI,1.13-1.90;P=0.004)、复合心血管转归(HR,1.74;95%CI,1.26-2.41;P=0.001)、非致命性心肌梗死(HR,1.73;95%CI,1.15-2.59;P=0.008)和非致死性中风(HR,2.67;95%CI,1.26-5.63;P=0.01)的风险显著增加相关。
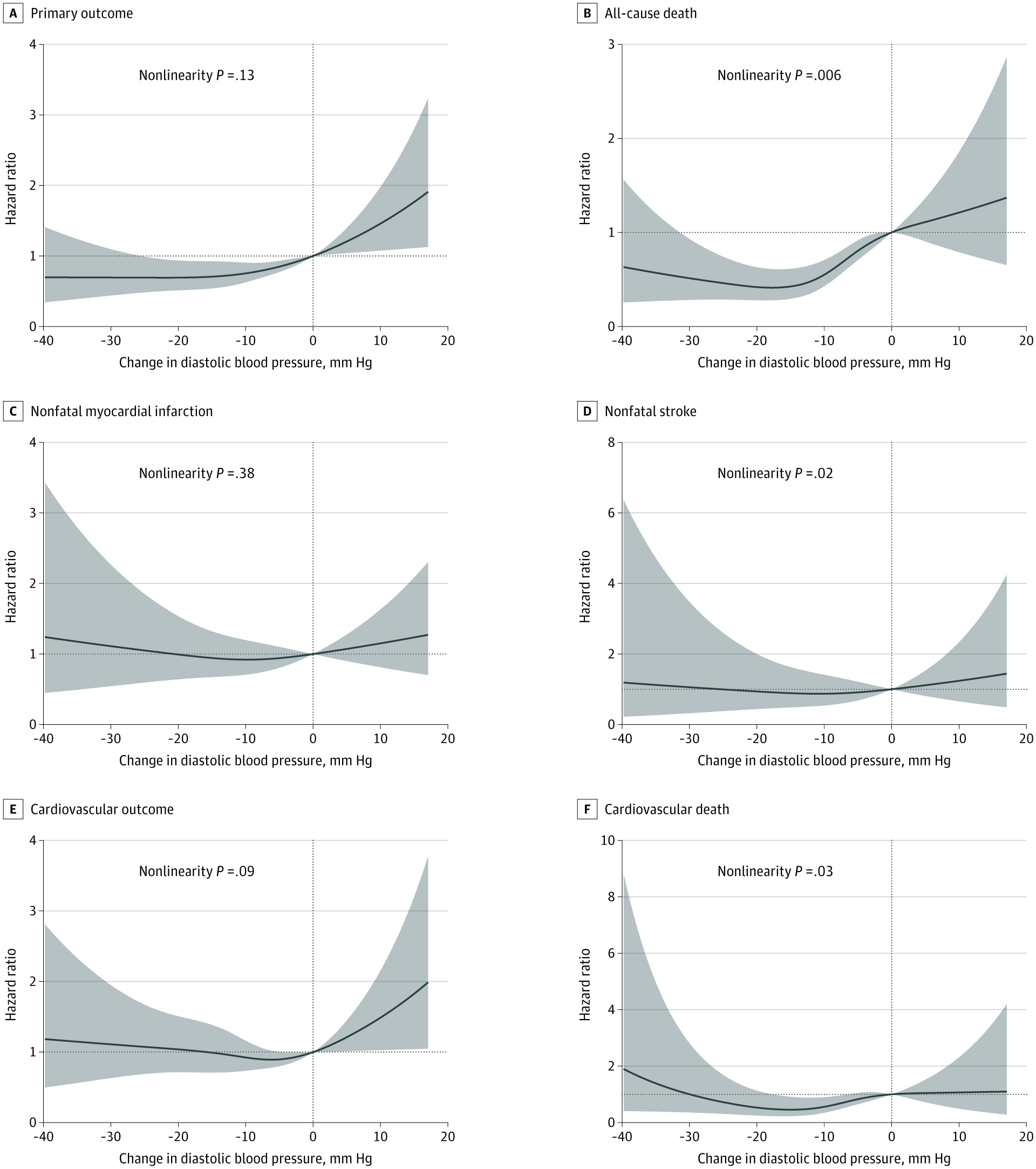
DBP值为80 mmHg作为参考。观察到经治疗的舒张压与主要结局(P = 0.003)、全因死亡(P = 0.001)和非致死性心肌梗死(P = 0.049)之间的非线性关系。
虽然没有观察到强化降压和基线舒张压之间的相互作用,但结果仍然迫使我们反思,降收缩压治疗潜在的额外好处是否可以抵消舒张压降至60mmHg以下的潜在风险。如果收缩压已经达到目标水平怎么办?使用SPRINT和ACCORD-BP的综合数据,研究者发现,与将舒张压降至70-80mmHg相比,将舒张压降至60mmHg以下与收缩压低于130mmHg的患者心血管风险增加46%相关,提示即使SBP达到目标水平,也存在舒张J形现象。DBP值在70到80mmHg之间是这个患者群体的最佳目标,这一发现值得考虑和进一步研究。
参考文献:Li J, Somers VK, Gao X, et al. Evaluation of Optimal Diastolic Blood Pressure Range Among Adults With Treated Systolic Blood Pressure Less Than 130 mm Hg. JAMA Netw Open. 2021;4(2):e2037554. doi:10.1001/jamanetworkopen.2020.37554
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
27
#收缩压#
42
#PE#
34
好文感谢分享
53
#舒张压#
48
好文
89
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
58
好文章!
86