Science:挑战常规!少突胶质细胞多样性远超想象
2016-06-10 佚名 生物谷
根据一项新的研究,少突胶质细胞(oligodendrocyte)---一种在多发性硬化症等疾病中发挥着至关重要作用的脑细胞---要比之前所认为的更加多样化。这一发现将有助我们理解这些细胞受到影响的疾病,并且可能为未来的治疗策略提供线索。相关研究结果发表在2016年6月10日那期Science期刊上,论文标题为“Oligodendrocyte heterogeneity in the mouse

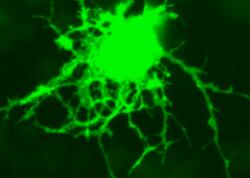
根据一项新的研究,少突胶质细胞(oligodendrocyte)---一种在多发性硬化症等疾病中发挥着至关重要作用的脑细胞---要比之前所认为的更加多样化。这一发现将有助我们理解这些细胞受到影响的疾病,并且可能为未来的治疗策略提供线索。相关研究结果发表在2016年6月10日那期Science期刊上,论文标题为“Oligodendrocyte heterogeneity in the mouse juvenile and adult central nervous system”。
在多发性硬化症和类似的神经疾病中,大脑中的电信号传送更加缓慢。这种下降的电信号传送速度导致麻木、平衡和行走困难、视力模糊等症状。多发性硬化症的特征是髓磷脂(myelin)---一种隔离神经细胞和允许电信号在大脑中快速传送的保护性髓鞘---丢失。髓磷脂是由少突胶质细胞产生的。尽管少突胶质细胞在此之前一直被认为一种同质的细胞群体,但是当前的这项研究给出一种不同的看法。
在论文通信作者Gonçalo Castelo-Branco博士和Sten Linnarsson博士的领导下,研究人员使用最近开发出的一种单细胞RNA测序技术。这种方法允许研究人员了解单个细胞中的基因活性。通过这种方式,他们能够揭示出利用传统方法可能无法可视化观察到的细胞之间的差异。研究人员分析了来自年轻小鼠和成年小鼠大脑几个部位和脊髓的5000多个少突胶质细胞,这允许他们前所未有详细地和清晰地观察这些细胞的多样性。
来自瑞典卡罗琳斯卡医学院医学生物化学与生物物理学系的Sten Linnarsson说,“我们意料之外地发现少突胶质细胞群体中的多样性。在这项研究中,我们鉴定出12个少突胶质细胞亚类型和一种新的与驻留在血管中的少突胶质细胞截然不同的细胞。”
他们发现在少突胶质细胞的发育过程中,它们成熟的初始阶段在年轻小鼠的中枢神经系统中是类似的,然而不同的成熟少突胶质细胞亚群富集在成年小鼠大脑中的特定区域中。
也来自卡罗琳斯卡医学院医学生物化学与生物物理学系的Gonçalo Castelo-Branco说,“发现这种意料之外的少突胶质细胞多样性可能让人们对多发性硬化症等神经疾病产生新的认识。”
原始出处
Sueli Marques1,*, Amit Zeisel1,*, Simone Codeluppi1,2, David van Bruggen1, Ana Mendanha Falcão1, Lin Xiao3,4, Huiliang Li3, Martin Häring1, Hannah Hochgerner1, Roman A. Romanov1,5, Daniel Gyllborg1, Ana B. Muñoz-Manchado1, Gioele La Manno1, Peter Lönnerberg1, Elisa M. Floriddia1, Fatemah Rezayee1, Patrik Ernfors1, Ernest Arenas1, Jens Hjerling-Leffler1, Tibor Harkany1,5, William D. Richardson3, Sten Linnarsson1,†, Gonçalo Castelo-Branco.Oligodendrocyte heterogeneity in the mouse juvenile and adult central nervous system.Science.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#少突胶质细胞#
29
#SCIE#
39
#胶质细胞#
34
#多样性#
36
很有意义的发现
105
自然精品
89
很好的发现
132