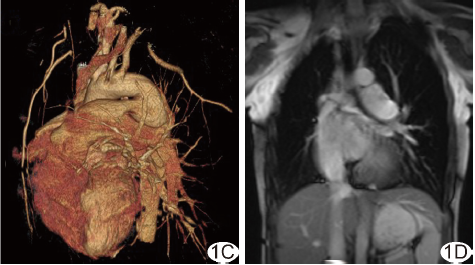
Radiology:心脏 MRI左心房功能评估预测心肌梗死后心血管事件的价值
2019-12-19 shaosai MedSci原创
背景:左心房(LA)功能在评估急性心肌梗死(AMI)的价值尚有争议。心脏MRI心肌特征识别(MRI-FT)是一种通过评估心肌功能来反应心房功能的一种方法。本研究旨在通过MRI-FT评估的LA功能与AMI后主要不良心血管事件(MACE)的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管事件#
43
#左心房#
51
#左心房功能#
54
#心房#
46
学习
91
学习了
76