顽固性低钠血症的原因终于找到了,罪魁祸首竟然是它!
2019-10-25 秦捷、李秀慧 中国护理管理
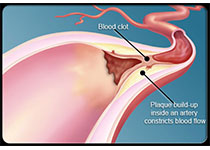
患者,老年女性,2小时前无明显诱因突然出现头痛,意识进行加重直至昏迷,呕吐大量胃内容物,行颅脑CT示蛛网膜下腔出血,以"蛛网膜下腔出血"于2019.7.23收入神经外科;于7.24行脑血管造影术+动脉瘤栓塞术;术后转入ICU继续治疗;患者于7.29由ICU转入我科。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#顽固性#
38
#低钠血症#
38
#低钠#
46
好
99
学习学习学习
91
好好好好好好
96