JAHA:TAVR后的冠脉造影评估TAVR-in-TAVR术后冠脉通路受损的风险
2020-06-25 xiangting MedSci原创
目前接受TAVR治疗的患者中,超过30%在TAVR-in-TAVR后冠脉通路不可用。
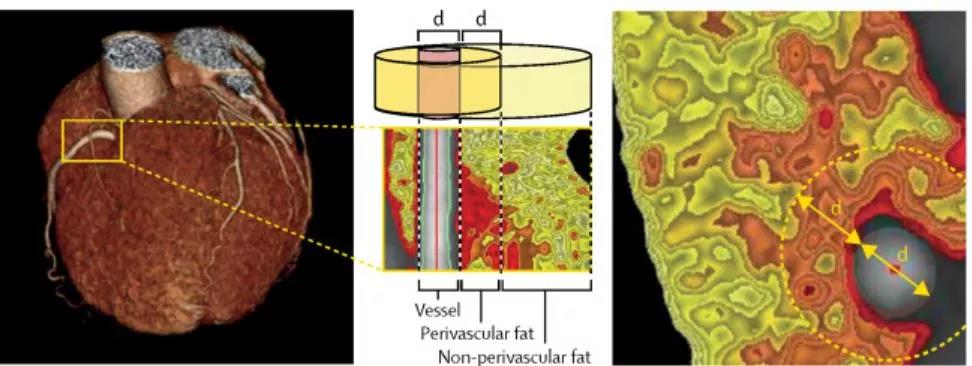
经导管主动脉瓣置换术(TAVR)后再次进行TAVR(TAVR-in-TAVR)是一种治疗经导管心脏瓣膜(THV)退化的方法。然而,首个THV的移位小叶会产生一个风险平面(RP),冠脉导管无法在该风险平面下通过。这项研究目的是评估TAVR-in-TAVR后冠脉通路(CA)受损的潜在风险。
对使用不同THVs进行TAVR后的137例连续性患者进行了前瞻性冠脉造影,观察导管穿过瓣膜框架的位置。如果冠脉插管是从RP下方通过的,则通过主动脉造影测量瓣膜框架与主动脉壁之间的距离。TAVR-in-TAVR后的CA定义为:如果导管从RP上方通过,则为可行;如果从RP下方通过,且瓣膜到主动脉的距离>2mm,则为理论上可行;如果从RP下方通过,且瓣膜到主动脉的距离≤2mm,则为不可行。
72名患者(53%)使用Sapien 3 THV,26名(19%)使用Evolut Pro/R THV,39名(28%)使用Acurate Neo THV。TAVR-in-TAVR后的CA被认为在40.9%的患者中可行(分别为68.1%、19.2%和5.1%,P<0.001),27.7%理论上可行(分别为8.3%、42.3%和53.8%,P<0.001),31.4%不可行(分别为23.6%、38.5%和41.1%,P=0.116)。TAVR-in-TAVR后CA受损的独立预测因素为女性(比值比[OR],3.99;95% CI,1.07-14.86;P=0.040)、窦管结直径(OR,0.62;95% CI,0.48-0.80;P<0.001)、瓣环上THV植入(OR,6.61;95% CI,1.98-22.03;P=0.002)。
目前接受TAVR治疗的患者中,超过30%在TAVR-in-TAVR后冠脉通路不可用。窦管结小和接受瓣环上THV的患者在TAVR-in-TAVR中潜在CA受损的风险最高。
原始出处:
Luca Nai Fovino. Coronary Angiography After Transcatheter Aortic Valve Replacement (TAVR) to Evaluate the Risk of Coronary Access Impairment After TAVR‐in‐TAVR. JAHA. 24 June 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TAVR#
69
#AVR#
29
#AHA#
27
#冠脉造影#
56
#造影#
34