Acta Neuropathologica: 多组分子图谱揭示了脑转移多种组织学共有的潜在靶向异常
2021-01-28 MedSci原创 MedSci原创
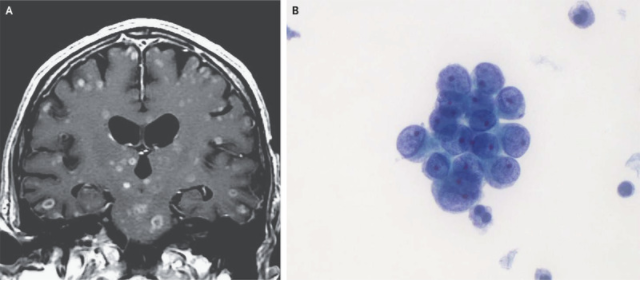
脑转移(BM)是系统性恶性肿瘤的一种常见且致命的并发症,常发生在10-30%的成年癌症患者中。手术入路和药物在中枢神经系统(CNS)内渗透的固有局限性进一步使BM的治疗复杂化。
脑转移(BM)是系统性恶性肿瘤的一种常见且致命的并发症,常发生在10-30%的成年癌症患者中。手术入路和药物在中枢神经系统(CNS)内渗透的固有局限性进一步使BM的治疗复杂化,并且随着原发性或其他颅外部位播散性恶性肿瘤治疗的不断改进,这些限制变得更加具有临床相关性。BM最常见于相对狭窄的肿瘤横切面,主要包括肺癌、乳腺癌和肾癌以及恶性黑色素瘤等,这表明在常见的脑转移肿瘤类型中,共有的生物学机制起着基础性作用。
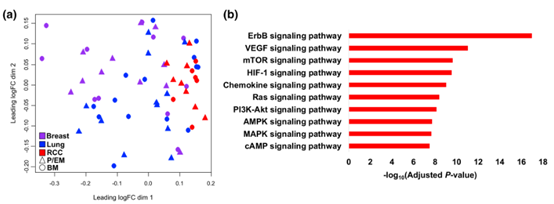
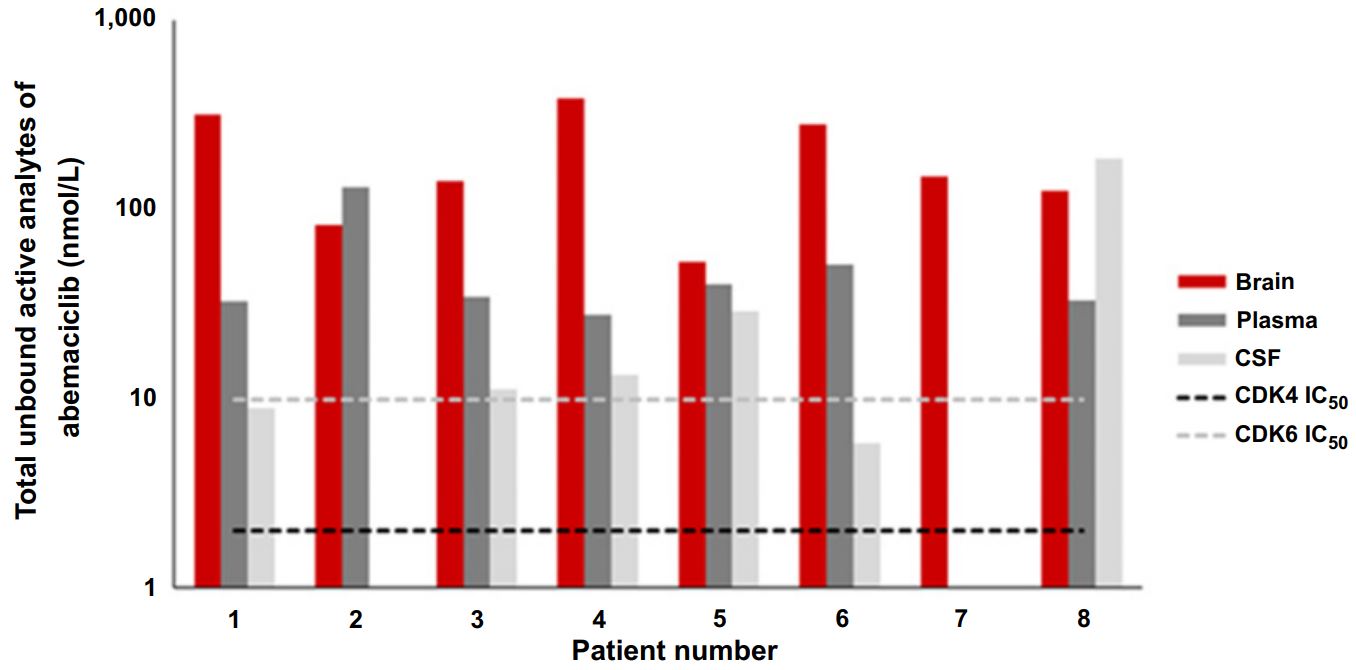
为了确定和描述这些机制,本研究使用全外显子组测序、mRN-seq和反相蛋白阵列分析对肺癌、乳腺癌和肾细胞癌(包括BM和患者匹配的原发性或颅外转移组织)进行了基因组、转录和蛋白质组学分析。虽然没有特定的基因组改变与BM相关,但在多种肿瘤组织学中,与细胞免疫受损、氧化磷酸化上调(OXPHOS)和包括磷酸肌醇3激酶(PI3K)信号在内的典型致癌信号通路的相关性是明显的。
多重免疫荧光分析证实BM中存在显著的T细胞耗竭,这表明免疫微环境发生了根本性的改变。此外,利用体外和体内模型进行的功能研究表明,与同基因亲本相比,小鼠BM模型和脑转移衍生物中的氧化代谢增强,对OXPHOS抑制敏感。
综上所述,致癌信号、细胞代谢和免疫微环境的病理生理学重组是BM的广泛特征。对这一生物学进一步分析阐明将可能揭示针对多种全身性癌症引起的BM的治疗开发的有希望的靶点。
Fukumura, K., Malgulwar, P.B., Fischer, G.M. et al. Multi-omic molecular profiling reveals potentially targetable abnormalities shared across multiple histologies of brain metastasis. Acta Neuropathol (2021). https://doi.org/10.1007/s00401-020-02256-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#分子图谱#
27
#组织学#
28
#Pathol#
31
#pathologic#
28
#CTA#
32