早应用早达标:伴多支病变的ASCVD极高危患者血脂管理的新观点
2019-06-10 国际循环编辑部 国际循环
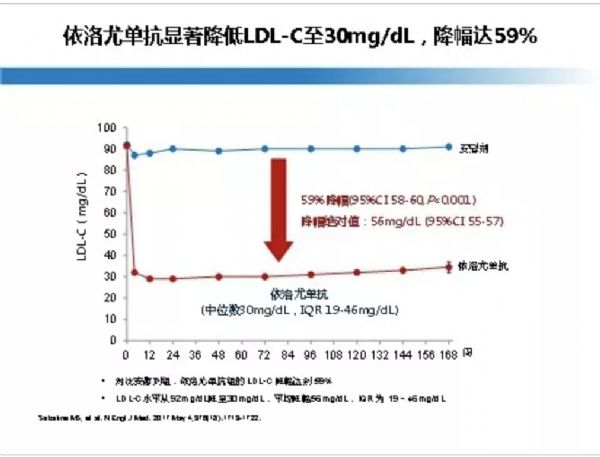
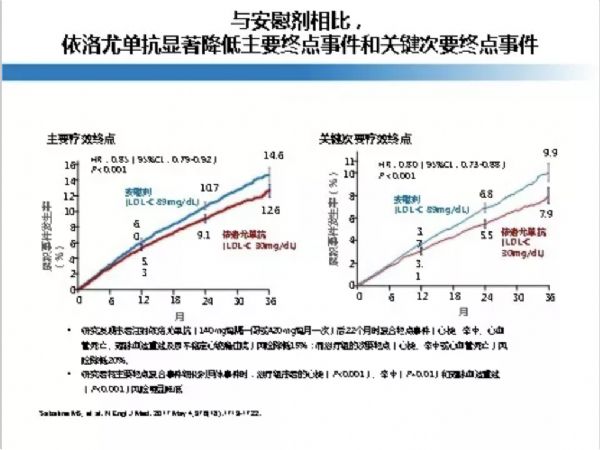
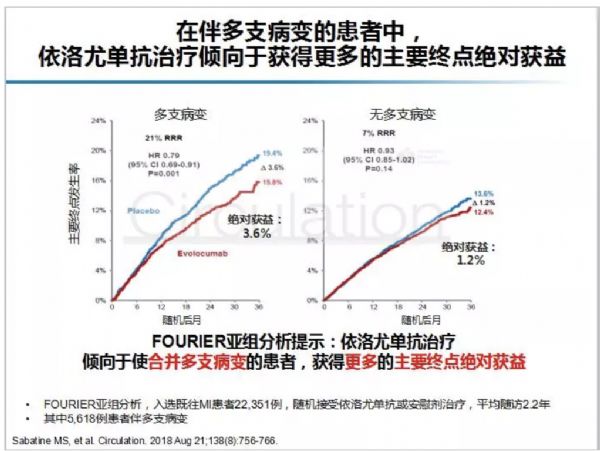
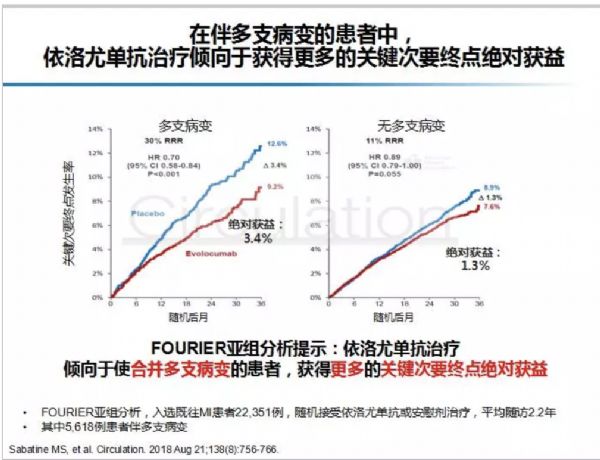
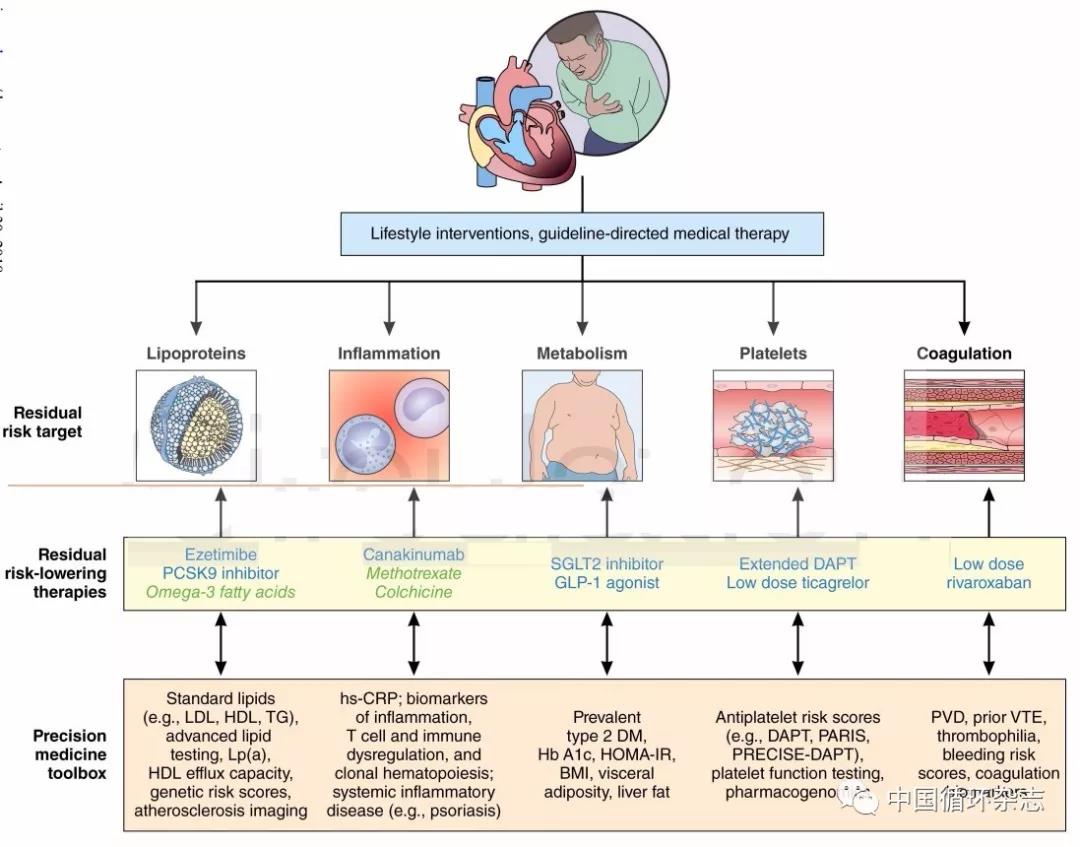
近期,国内外一些新的指南,在ASCVD患者中推荐进一步对风险高低进行划分,其中合并多支病变就被认为是ASCVD中的极高风险。在本届东方心脏病学会议上,来自上海第六人民医院的魏盟教授就伴多支病变的ASCVD极高危患者如何有效管理血脂水平发表了新的观点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高危患者#
48
#ASC#
43
怎么找到参考文献呢
78
好
70
#ASCVD#
52
学习
77
学习学习学习
79