Neurology:Occrelizumab在不同类型的多发性硬化症患者中的安全性
2021-09-08 Nebula MedSci原创
Ocrelizumab 在复发性或原发性进行性多发性硬化症患者中长期使用的安全性良好
Ocrelizumab(OCR)是一种人源化的抗CD20 单克隆抗体,可选择性地靶向CD20阳性B细胞。CD20阳性B细胞被认为是导致髓鞘和轴突损伤的关键因素,这种神经损伤可导致多发性硬化症(MS)患者残疾。
目前,Ocrelizumab 已获得了FDA批准用于治疗多发性硬化症。本文报告了 Ocrelizumab 用于复发性多发性硬化症(RMS)和原发性进行性多发性硬化症患者长达7年的安全性。
安全性分析是基于11项临床试验(包括2期、3期和3b期试验)中接受 Ocrelizumab 治疗的所有患者的综合临床和实验室数据。对于选定的不良事件(AEs),使用额外的上市后数据。使用多种流行病学资料对严重感染 (SI) 和恶性肿瘤的发病率进行分析。
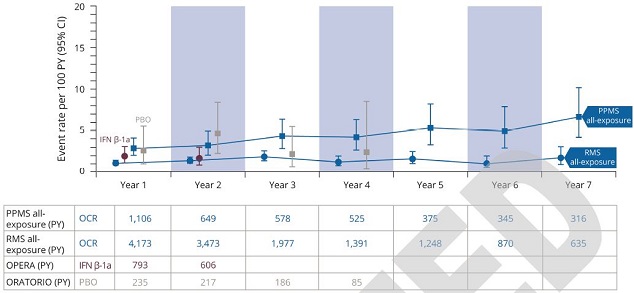
严重感染的年发生率
截止2020年1月时,共有5680位多发性硬化症患者接受了 Ocrelizumab 治疗(共暴露了18218个患者·年[PY])。在接受 Ocrelizumab 治疗的患者中,不良事件(AE)的发生率为 248 例/100 患者·年(范围 246-251),严重 AE、输液相关反应和感染的发生率分别是 7.3(7.0-7.7)、25.9(25.1-26.6)和 76.2(74.9-77.4)/100 患者·年;在3期试验治疗过程中,Ocrelizumab组的不良事件发生率与对照组的相近。最常见的严重 AE(包括 SI 和恶性肿瘤)的发生率与流行病学数据报告的范围一致。
综上,无论是在临床试验中持续使用长达 7 年,还是在现实世界中广泛使用超过 3 年,Ocrelizumab 在复发性或原发性进行性多发性硬化症患者中的安全性均良好。
原始出处:
Hauser Stephen L,Kappos Ludwig,Montalban Xavier et al. Safety of Ocrelizumab in Patients With Relapsing and Primary Progressive Multiple Sclerosis.[J] .Neurology, 2021, https://doi.org/10.1212/WNL.0000000000012700
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#硬化症#
35
#Neurol#
30
#多发性#
33
#不同类型#
46
#mAb#
38
#OCC#
29
#CRE#
47
哦靠天咯是咯矿咯啊伏特加
56
学习学习
61
Ocrelizumab(OCR)是一种人源化的抗CD20 单克隆抗体,可选择性地靶向CD20阳性B细胞。
59