Diabetes Obes Metab:1型糖尿病成人血糖快速升高可降低心率变异性
2020-12-12 MedSci原创 MedSci原创
1型糖尿病患者的HRV在不同血糖范围内均无明显变化。HRV取决于葡萄糖的变化速率,尤其是血糖快速升高。
近日,代谢内分泌疾病领域权威杂志Diabetes Obesity & Metabolism上发表了一篇研究文章,这项研究旨在调查1型糖尿病患者不同血糖浓度的口服葡萄糖耐量测试(OGTT)期间心率变异性(HRV)的差异。
这项单中心、前瞻性、次要结局分析是在17名1型糖尿病(HbA1c为7.0±0.6%)患者中进行,他们接受了两次OGTT(禁食12到36小时后),以调查快速血糖波动和OGTT期间不同血糖范围反应后HRV的差异。
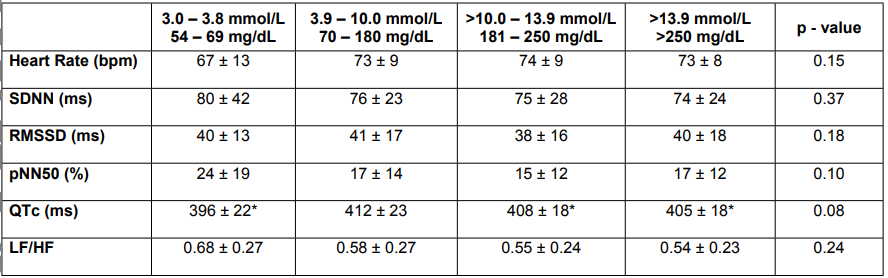
根据葡萄糖的变化,心率(p<0.001)、全程相邻NN间期之差的均方根值(RMSSD)(p=0.002)和QTc(p=0.04)发生了显著变化,血糖快速升高期间HRV降低尤其明显。OGTT期间的血糖波动对HRV没有影响(p<0.05)。
由此可见,1型糖尿病患者的HRV在不同血糖范围内均无明显变化。HRV取决于葡萄糖的变化速率,尤其是血糖快速升高。
原始出处:
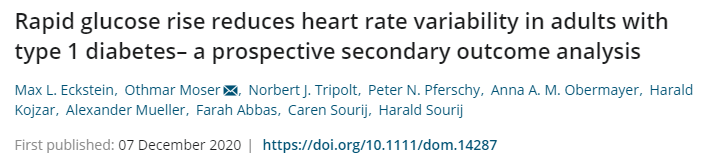
Max L. Eckstein.et al.Rapid glucose rise reduces heart rate variability in adults with type 1 diabetes– a prospective secondary outcome analysis.Diabetes Obesity & Metabolism.2020.https://doi.org/10.1111/dom.14287
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Diabetes#
32
#MET#
39
#DIA#
39
#Meta#
28
#BET#
29
受教
71
#变异#
26
#心率变异性#
39
谢谢MedSci提供最新的资讯
48