Environ Res:吸烟、环境烟草烟雾、室内粉刷和居住在新旧建筑中对哮喘、鼻炎和呼吸道症状影响情况的前瞻性研究
2020-10-24 AlexYang MedSci原创
最近,有研究人员对北欧11506名成年人进行了为期10年的跟踪调查,探索了烟草烟雾、家庭环境和呼吸系统健康之间的关系。
最近,有研究人员对北欧11506名成年人进行了为期10年的跟踪调查,探索了烟草烟雾、家庭环境和呼吸系统健康之间的关系。
研究人员使用了多层次逻辑回归模型用于评估症状的发生和缓解情况。基线时吸烟者会出现更多的呼吸道症状(OR=1.39-4.43)和鼻炎症状(OR=1.35)。随访期间开始吸烟者能够增加新的呼吸道症状的风险(OR=1.54-1.97);而戒烟能够降低风险(OR=0.34-0.60)。基线时的ETS增加了喘息的风险(OR=1.26)。基线或随访时加上ETS时会增加喘息(OR=1.27)和夜间咳嗽(OR=1.22)的风险。基线时的木器涂装会降低哮喘的缓解(OR 95%CI:0.61,0.38-0.99)。家里的地板涂装增加了排痰性咳嗽(OR 95%CI:1.64,1.15-2.34),并降低喘息的缓解(OR 95%CI:0.63,0.40-0.996)。室内涂装(OR 95%CI:1.43,1.16-1.75)和地板涂装(OR 95%CI:1.77,1.11-2.82)能够增加过敏性鼻炎的缓解。住在最老的建筑(1960年以前建造)与较高的夜间咳嗽和医生诊断哮喘的发病率有关。住在最新的建筑(1986-2001年建造)与较高的夜间呼吸困难(OR=1.39)和鼻炎(OR=1.34)发病率有关。
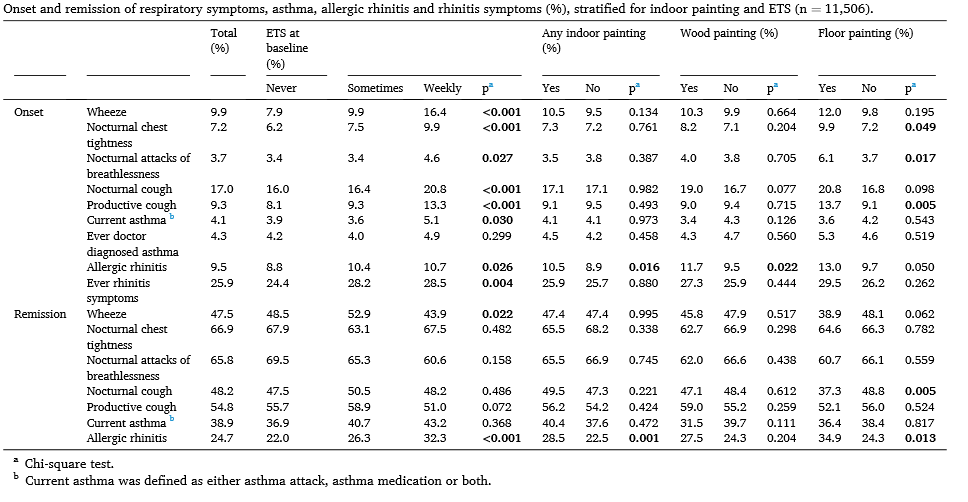

最后,研究人员指出,吸烟、ETS和室内粉刷是呼吸道症状的风险因素。木器涂装和地板涂装能够降低呼吸道症状的缓解。吸烟可增加鼻炎风险。住在旧楼房是夜咳和医生诊断哮喘的风险因素,而住在新楼房会增加夜间呼吸困难和鼻炎风险。
原始出处:
Juan Wang , Christer Janson , Rain Jogi et al. A prospective study on the role of smoking, environmental tobacco smoke, indoor painting and living in old or new buildings on asthma, rhinitis and respiratory symptoms. Environ Res. Sep 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#呼吸道症状#
39
#前瞻性#
35
#前瞻性研究#
34
#呼吸道#
38
#烟草#
0
#iron#
35
身体素质高这些都不怕
87