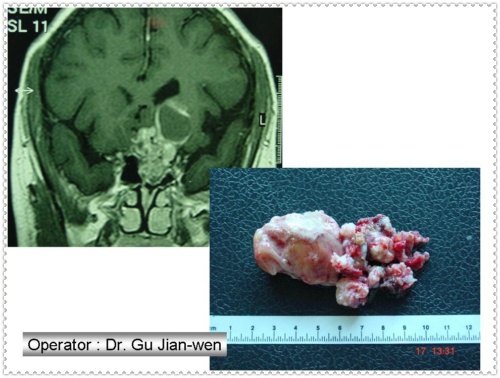
颅咽管瘤生长部位与下丘脑结构关系密切,部分肿瘤常与垂体柄、漏斗、内侧隆起粘连,虽然肿瘤呈良性生长,但常规手术全切肿瘤很困难,常出现严重并发症,如尿崩、水电解质紊乱等。我们采用显微外科技术,经改良翼点入路及鞍区的4个解剖间隙充分显露和切除肿瘤,路径最短。在手术显微镜、放大及照明下能够解剖出与视神经、视交叉及下丘脑或颈内动脉等粘连处,肿瘤全切后,解剖结构保留完整,术后并发症轻,愈后良好。
nbsp; 手术过程 病人均在全麻下取仰卧头偏左转30°,以右侧过中线改良翼点入路切口,骨瓣尽量低,以减少对脑的牵拉,剪开侧裂池,经前床突内侧颈内动脉起始,探查视交叉前、视神经外侧、颈内动脉外侧间隙,从间隙肿瘤推移明显或突出处分离肿瘤,先行肿瘤囊液吸出或囊内取瘤。随着瘤体缩小,从肿瘤表面与周围组织结构分界面即蛛网膜下腔层仔细分开,电凝仅限用于供给肿瘤的细小动脉,应避免颈内动脉、后交通动脉、大脑前动脉、前交通动脉及其发出下丘脑穿动脉、垂体上动脉的损伤。碎块切除肿瘤,直至肿瘤全切,对与肿瘤粘连紧密的垂体柄、漏斗,内侧隆起和灰结节等结构应在高倍镜下辨认,仔细分离。凸入三脑室的肿瘤随着肿瘤的缩小,而逐渐下陷,略轻牵拉即可切除。由于颅咽管瘤生长部位特殊,其周围解剖结构复杂。全切肿瘤一定要严格遵守显微神经外科操作,在良好的显微镜下进行。一般情况下肿瘤与周围结构多形成边界即蛛网膜界面,分离肿瘤时,应循肿瘤表面进行,对与肿瘤粘连紧密的垂体柄、漏斗、内侧隆起和灰结节等结构应在高倍镜下辨认,仔细分离,对于因肿瘤生长,压迫变形的垂体柄,可从垂体柄表面的静脉髓纹来判断。即使术中分离肿瘤时垂体柄断裂,也要谨慎地把肿瘤与垂体柄分离,保留残存的垂体柄完整,有利于术后下丘脑功能的恢复。
颅咽管瘤的供血动脉来自Wills环各段的穿通动脉,术中除防止Wills环构成的动脉大血管损伤外,还应保持细小穿通动脉的供血,对减轻术后并发症非常重要。切开终板入路时,应避免损伤前交通动脉及其穿通支,特别注意Heubmers动脉损伤,它分布在尾状核头,内囊1/3前穿质;从视交叉前间隙取瘤时,应注意颈动脉发出至垂体柄、漏斗、内侧隆起和灰结节结构的垂体上动脉损伤。从视神经外侧间隙取瘤时,除要防止垂体上动脉损伤外,尚有从后交通动脉至乳头体、灰结节、视交叉和旁穿支等结构的旁穿支穿动脉。从大脑后动脉和基底动脉发出丘脑穿通动脉供给后穿支,脚间窝部分,多不参与肿瘤供血,这些与中脑网状结构,锥体束和脊髓丘脑束功能密切相关的穿通动脉,在切除后上部肿瘤时应给予特别的注意。此外,术中这些动脉过度伸拉和暴露较长时可发生血管痉挛产生这些穿通动脉缺血.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#切除术#
26
值得学习
97
#颅咽管瘤#
40