PNAS:苹果皮中的化合物可逆转多发性硬化症中的神经元损伤
2020-04-12 网络 网络
《PNAS》上的一项新研究表明,在苹果、李子等水果的果皮和一些草药中发现的一种化合物熊果酸,可以减少对神经元的进一步损害,还有助于重建覆盖神经元的保护鞘,从而逆转这种损害。
多发性硬化症(MS)的特征是肌肉无力和麻痹加剧,有多种疗法可在早期帮助延缓疾病的进展,但很难逆转已经发生在神经元中的损伤。《PNAS》上的一项新研究表明,在苹果、李子等水果的果皮和一些草药中发现的一种化合物熊果酸,可以减少对神经元的进一步损害,还有助于重建覆盖神经元的保护鞘,从而逆转这种损害。
研究人员使用了实验室级别的熊果酸纯化物进行实验,他们利用一种已建立的多发性硬化症小鼠模型EAE,该模型模仿人类疾病,在其生命过程中缓慢发展疾病,大约在第12天,MS的迹象、部分麻痹的出现以及当前可用的药物最有效时,小鼠即开始疾病的急性期。
研究人员在第60天疾病晚期时开始治疗小鼠,此时大脑和脊髓已经形成了慢性组织损伤,需要对其进行修复和再生。在治疗的第20天开始见好转,实验开始时瘫痪的小鼠在治疗后恢复了行走的能力,尽管有些虚弱。研究人员称,这虽然不是一种治愈的方法,但是如果在人身上看到类似的反应,那将代表生活质量的重大变化。而且最重要的是,这是一种逆转,是在疾病发展到如此晚的阶段从未见过的。
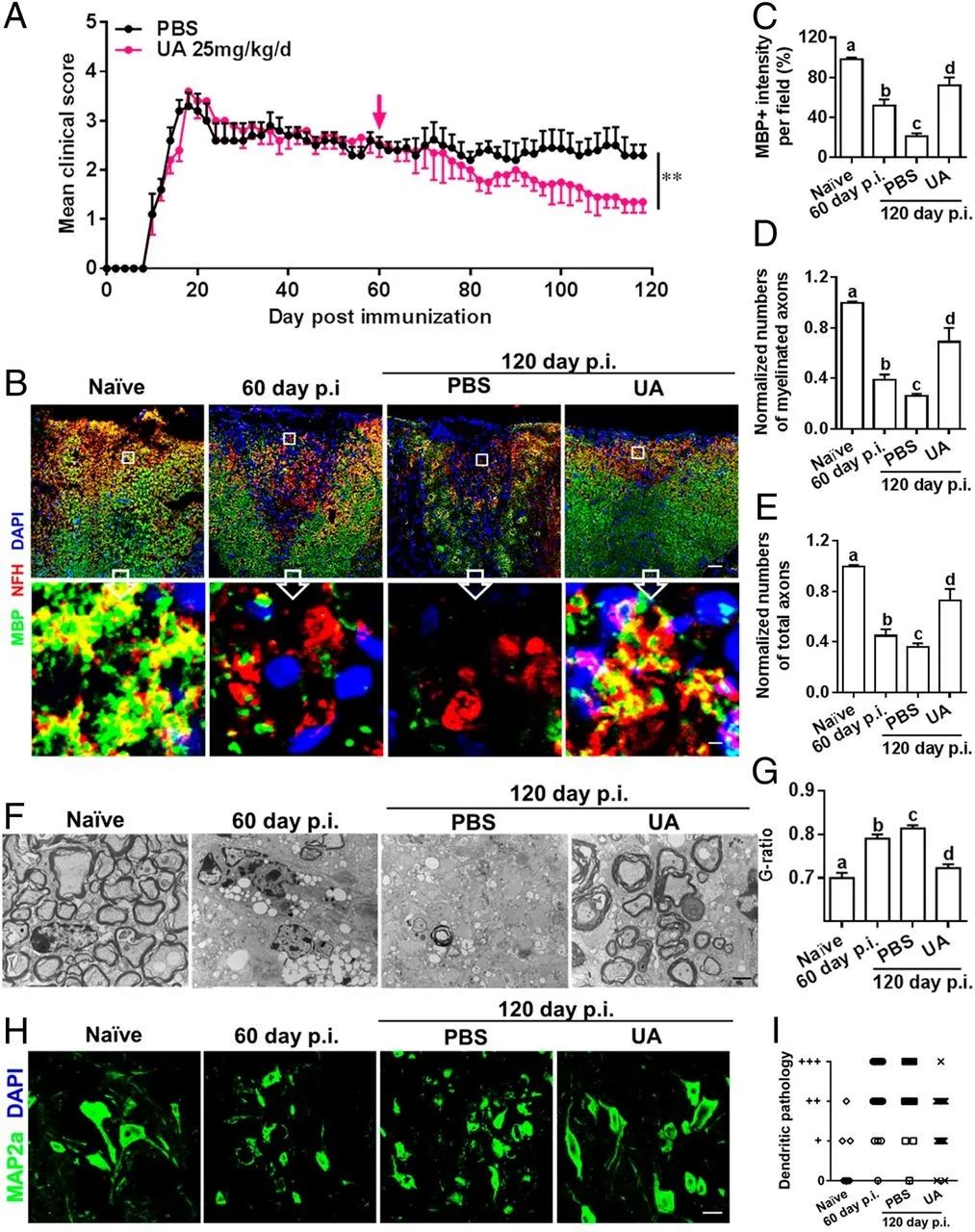
熊果酸治疗可缓解慢性EAE,促进髓鞘再生并减少轴突变性和神经元树突破坏
此外,研究人员还研究了熊果酸如何作用于细胞,他们观察到它抑制了Th17细胞,Th17细胞是一种免疫细胞,是MS病理自身免疫反应的主要驱动力之一。目前许多疗法似乎都抑制Th17,但是该化合物可以激活前体细胞,使其成熟成为急需的髓鞘生成细胞,即少突胶质细胞。这种成熟作用是最关键的,MS中制造髓鞘的少突胶质细胞耗尽,而产生新的少突胶质细胞的干细胞处于休眠状态,无法成熟。这种化合物有助于激活这些干细胞,可能就是症状逆转的原因。
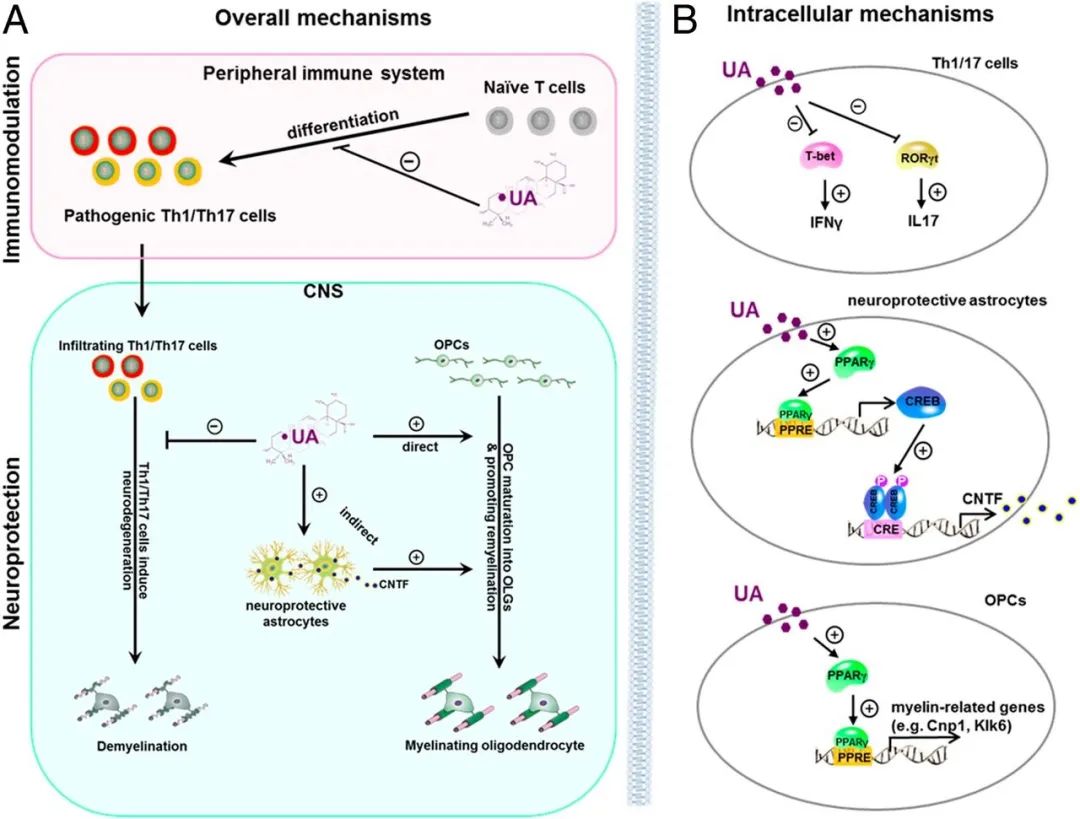
熊果酸介导的EAE免疫调节和神经再生作用模型
尽管来自动物疾病模型的证据是初步的,但在实验室中看到一种化合物既能中止又能修复多发性疾病的损伤,是令人鼓舞的。研究人员下一步计划测试化合物的安全性,在首次临床试验之前,仍有许多测试需要完成,这是治疗疾病的一个伟大的先导。
原始出处:
Yuan Zhang, et al. A dual effect of ursolic acid to the treatment of multiple sclerosis through both immunomodulation and direct remyelination. PNAS. first published April 6, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PNAS#
29
#硬化症#
25
#多发性#
26
#化合物#
43
#损伤#
29
#苹果#
43