JCEM:伴有和不伴有2型糖尿病的COVID-19住院患者炎症与死亡率的关系
2022-01-07 MedSci原创 MedSci原创
该研究的结果表明COVID19患者死亡率与血清中先天炎性细胞因子IL-6和炎性趋化因子IL-8和IP10的水平升高相关。
炎症在COVID-19免疫病理学和疾病严重程度中发挥着重要的作用。然而,炎症与COVID-19病例的严重程度和死亡率之间的相关性尚未明确。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究的目的是明确炎症与COVID-19住院患者死亡率之间的关系,并评估这种关联是否因2型糖尿病状态的层次而异。
研究人员对哥伦比亚大学欧文医学中心的538名COVID-19住院患者进行了病例对照(死亡-存活)研究,按糖尿病状态分层。研究人员采用免疫测定法量化了血清中八种细胞因子和趋化因子的水平,包括干扰素(IFN)-α2、IFN-γ、白细胞介素(IL)-1α、IL-1β、IL-6、IL-8/CXCL8、IFNγ诱导蛋白10(IP10)/CXCL10和肿瘤坏死因子α(TNF-α)。Logistic回归模型用于评估炎症标志物(或其主要成分)对数转换与死亡率之间的关系。
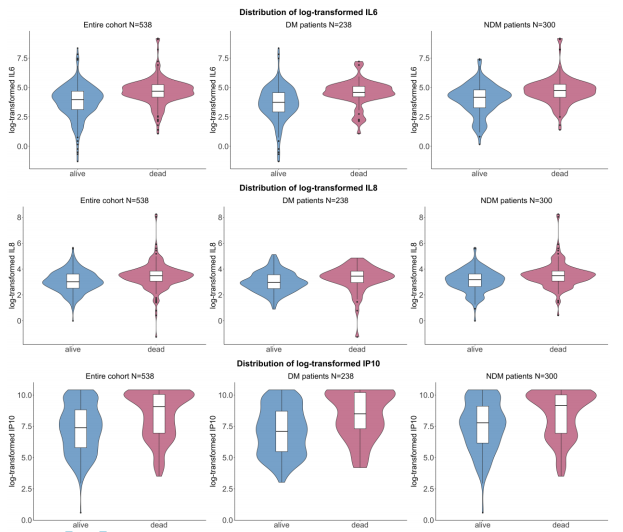
在多元Logistic回归模型中,血清中较高的IL-6(调整后的比值比(aOR)为1.74,95%置信区间(CI)为1.48-2.06)、IL-8(aOR为1.75(aOR为1.41-2.19))和IP10(aOR为1.36(1.24-1.51))水平与患者死亡率显著相关。在糖尿病的每一个分层中,研究人员也观察到了相同的炎症标志物与死亡率之间存在显著的正相关性。
由此可见,该研究的结果表明COVID19患者死亡率与血清中先天炎性细胞因子IL-6和炎性趋化因子IL-8和IP10的水平升高相关。这种关联在糖尿病各分层中是一致的,表明针对这些先天免疫途径的干预措施可让糖尿病患者受益。
原始出处:
Jia Guo.et al.Inflammation and mortality in COVID-19 hospitalized patients with and without type 2 diabetes.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac003/6499340
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
30
#JCEM#
36
学习学习
62
值得关注
54