Lancet respirat:同济大学3期临床试验揭示埃克替尼在EGFR突变型晚期NSCLC中的疗效
2021-07-19 MedSci原创 MedSci原创
与化疗相比,埃克替尼显著提高了NSCLC患者的无病生存期,并且具有更好的耐受性
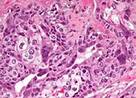
埃克替尼(Icotinib)为晚期表皮生长因子受体 (EGFR) 突变型非小细胞肺癌 (NSCLC) 患者提供了生存益处。EVIDENCE试验是一项在中国的29家医院开展的多中心、随机、开放标签的3期研究,旨在在肿瘤完全切除后的EGFR突变型II-IIIA期 NSCLC患者中比较埃克替尼与化疗的效果和安全性。本文报告了该研究预定的中期分析结果。
该研究招募了18-70岁的、组织学证实的II-IIIA期NSCLC患者,在随机分组前8周进行了肿瘤完全切除,且经检测在EGFR基因的19号或21号外显子上存在激活突变。受试者被随机(1:1)分至两组,接受口服埃克替尼(125 mg,3次/天)治疗2年,或静脉化疗(腺癌或鳞癌:长春瑞滨[25 mg/m2,第1天和8天] 联合 顺铂[75mg/m2,每个疗程的第1天];非鳞癌:培美曲塞[500 mg/m2] 联合 顺铂 [75 mg/m2,每3周的第1天])。主要终点是无病生存期。次要终点是总生存期和安全性。
生存预后
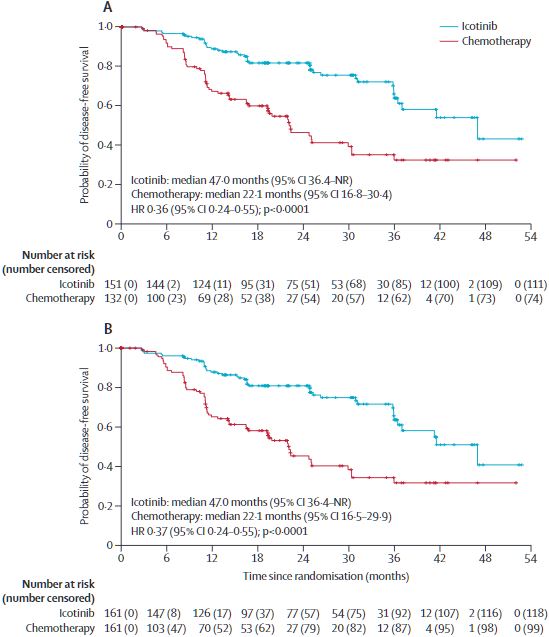
2015年6月8日至2019年8月2日期间,322位患者被随机分至埃克替尼组或化疗组(各151组);埃克替尼组151位患者和化疗组132位患者被纳入全分析队列。全分析队列的中位随访时间是24.9个月(IQR 16.6-36.4)。埃克替尼组的151位患者中有40位(26%)、化疗组的132位患者中有58位(44%)发生了疾病复发或死亡。埃克替尼组和化疗组的中位无病生存期分别是47.0个月(95%CI 36.4-未及)和22.1个月(16.8-30.4;校正风险比[HR] 0.36 [95%CI 0.24-0.55]; p<0.0001)。
埃克替尼组和化疗组的3年无病生存期分别是63.9%(95%CI 51.8-73.7)和32.5%(21.3-44.2)。总生存数据不成熟,埃克替尼组14例(9%)死亡,化疗组有14 例(11%)死亡。
埃克替尼组和化疗组分别有2位(1%)和19位(14%)患者发生了治疗相关的严重不良反应。两组均未观察到间质性肺炎或治疗相关死亡。
综上所述,本次分析结果表明,在肿瘤完全切除后的 EGFR突变的II-IIIA期NSCLC患者中,与化疗相比,埃克替尼显著提高了无病生存期,并且具有更好的耐受性。
原始出处:
Jianxing, et al. Icotinib versus chemotherapy as adjuvant treatment for stage II–IIIA EGFR-mutant non-small-cell lung cancer (EVIDENCE): a randomised, open-label, phase 3 trial. The Lancet Respiratory Medicine. July 16, 2021. https://doi.org/10.1016/S2213-2600(21)00134-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#同济大学#
41
#3期临床#
41
#Lancet#
46
#突变型#
32
#晚期NSCLC#
38
#埃克替尼#
35
#GFR#
34
#3期临床试验#
42
谢谢梅斯提供这么好的信息,学到很多
59
顶刊就是不一样,质量很高,内容精彩!学到很多
67