第十七届中国介入心脏病学大会(CIT2019)|于波:ST段抬高型心肌梗死冠状动脉内成像研究的新发现
2019-03-30 Vina MedSci原创
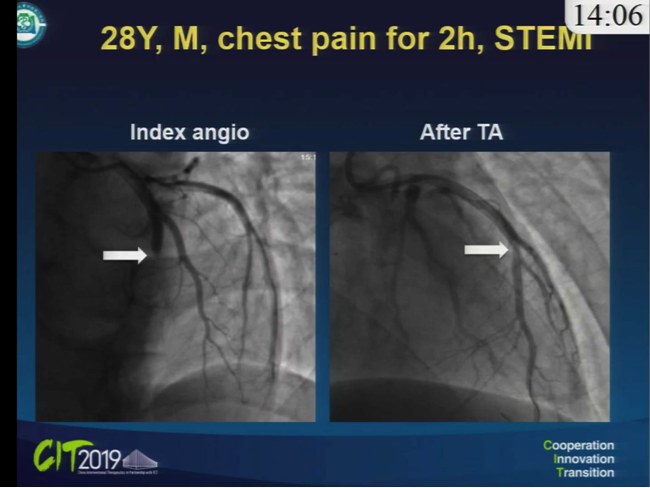
首先分享一个case。 28岁,男性,胸痛2h入院,心电图明确提示STEMI,冠脉造影提示:左前降支中段闭塞,右回旋支灌注良好,询问病史后唯一危险因素为吸烟。 对于类似病例,目前常规治疗方式为介入治疗、抗栓治疗或血栓抽吸后复查造影,实际上应尽量通过造影手段判断其栓塞机制。 ACS犯罪病变病理分类包括斑块破裂、侵蚀、钙化结节、夹层等,众多临床尸检结果显示斑块破裂占75%,斑块侵蚀占据1/3
首先分享一个case。
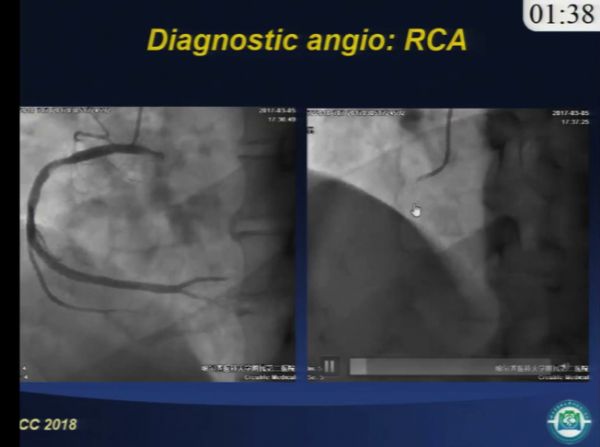
28岁,男性,胸痛2h入院,心电图明确提示STEMI,冠脉造影提示:左前降支中段闭塞,右回旋支灌注良好,询问病史后唯一危险因素为吸烟。
对于类似病例,目前常规治疗方式为介入治疗、抗栓治疗或血栓抽吸后复查造影,实际上应尽量通过造影手段判断其栓塞机制。
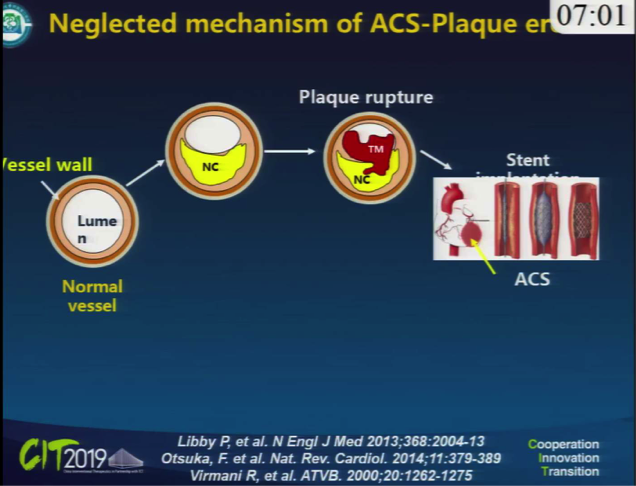
ACS犯罪病变病理分类包括斑块破裂、侵蚀、钙化结节、夹层等,众多临床尸检结果显示斑块破裂占75%,斑块侵蚀占据1/3,钙化结节不到10%。
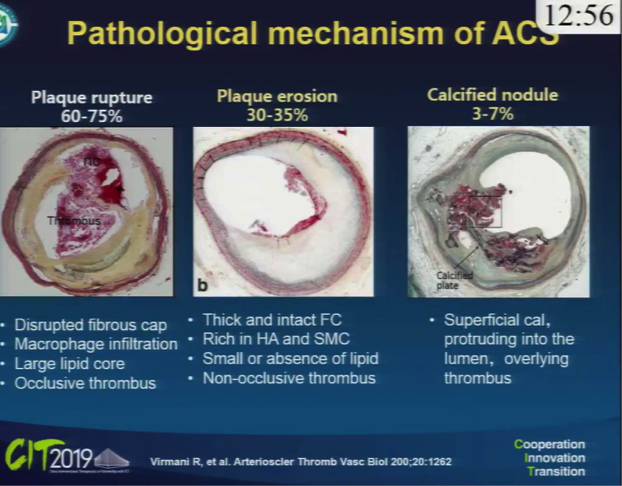
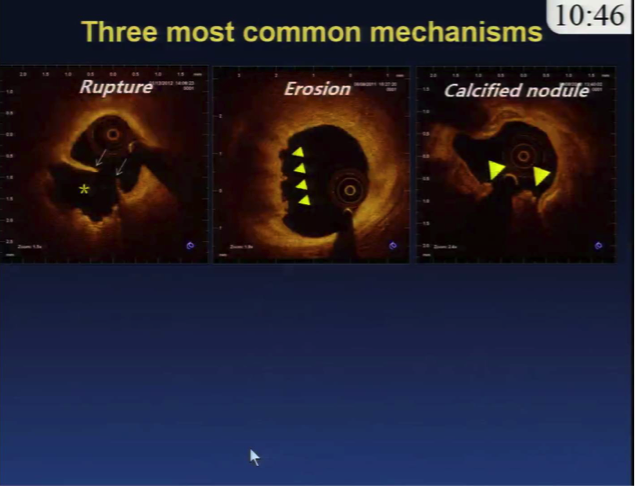
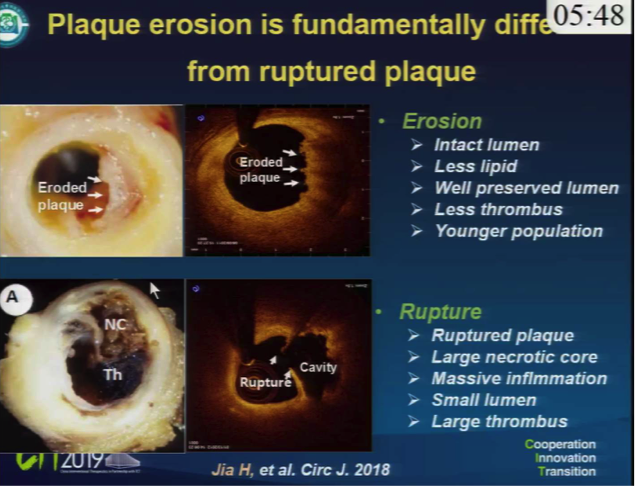
以下为对ACS犯罪病变的病理和影像学分类,ACS犯罪病变的影像学分类与病理分类一致。最常见的是斑块破裂,斑块破裂和钙化结节都存在纤维帽断裂。而斑块侵蚀为最难判断的类型,可通过排除其他类型进行诊断。
斑块侵蚀其多为非闭塞性血栓,影像表现多数管壁光滑而管腔大。
钙化结节多数前后弥漫钙化且突入到管腔,上面伴有血栓的形成。
ACS中斑块侵蚀大概占1/3,STEMI中斑块侵蚀大概占1/4。

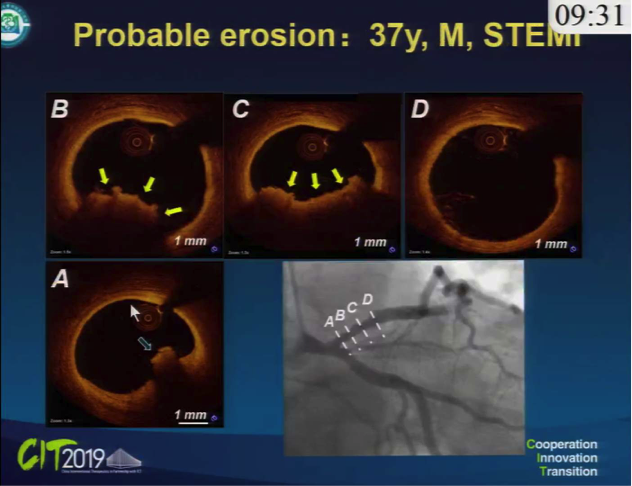
如下为几个比较典型的影像case。
破裂斑块影像上表现非常复杂。从近端到远端只有少量腹壁血栓,其他管腔非常好,基本是纤维斑块。
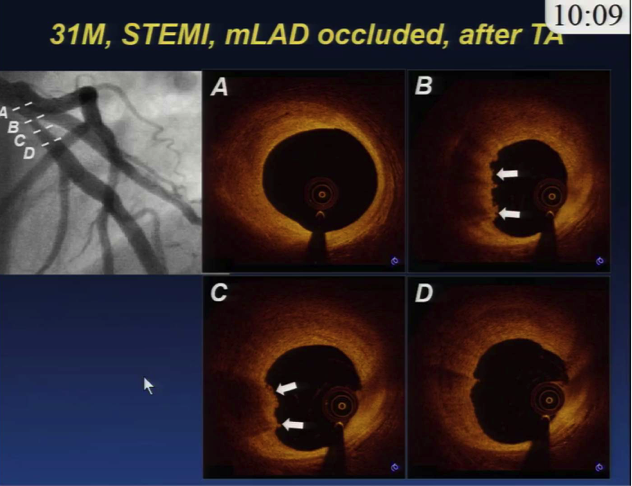
可能的斑块侵蚀,有大量血栓,尤其是红色血栓,OCT穿不透这种红色血栓,有大量红细胞。血栓周围基本是正常的管腔。
OCT上能看到的更多能导致ACS的病变。

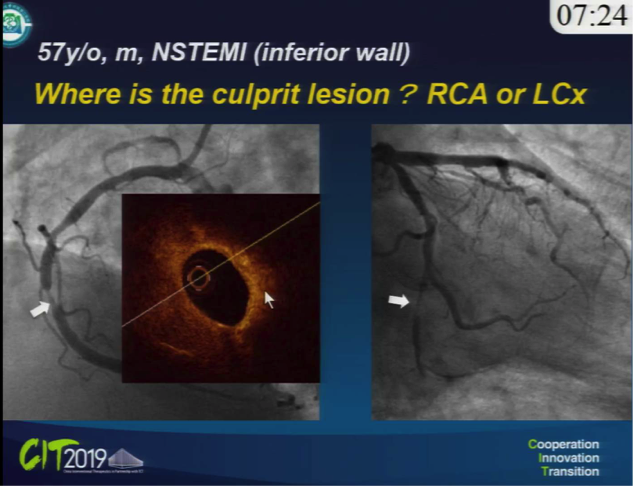
对于NSTEMI伴多支病变则较难确定其罪犯病变。
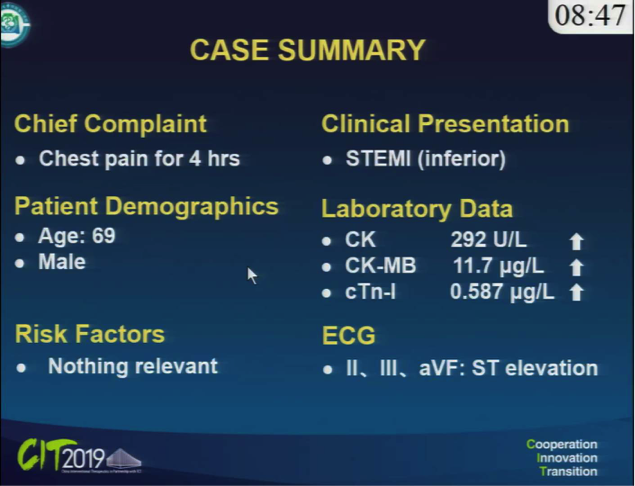
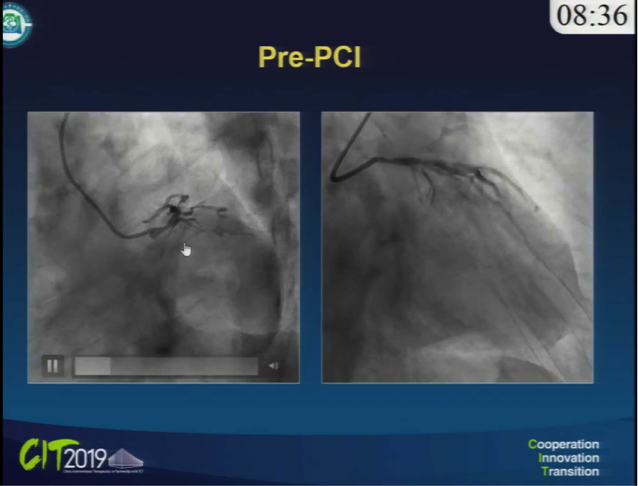
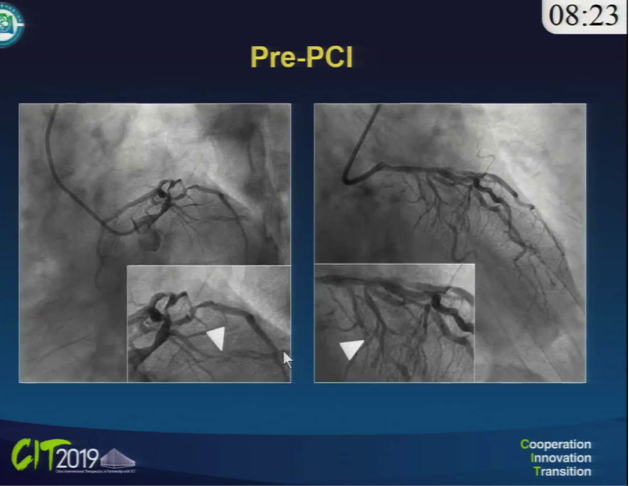
胸痛4个小时 69岁患者,明确下壁心梗。造影回旋支出口闭塞,远端有细微血流,基本是闭塞病变。右冠血流正常,有弥漫病变,没有明确固定的狭窄。近端有模糊、发白,像钙化或血栓,但血流正常。
首先考虑下壁,但右冠OCT发现,其实右冠是真正的罪犯病变。严重钙化,伴有脂质,出现斑块破裂,带有大量血栓。

57岁患者,NSTEI下壁,右冠病变80%,回旋支80%-90%狭窄,血流好。OCT右冠稳定斑块,真正的罪犯病变在回旋,非常大的脂质斑块,伴有斑块破裂。
处理罪犯病变时选择什么策略?
对动脉粥样硬化STEMI患者开通血管后,常规支架置入,置入后抗栓治疗、降脂治疗、抗炎治疗。
但有1/3的患者,尤其年轻患者,在溶栓或血流开通后没有明确好转。对于粥样斑块没有明确的推荐。
29例溶栓以后STEMI患者,发现抗栓治疗对斑块侵蚀的效果很好。

斑块侵蚀多数管腔完整,白色血栓,非闭塞型,多见于年轻患者,尤其是吸烟女性患者。
心脏骤停,造影远端闭塞。抗栓治疗后,远端管腔几乎正常。
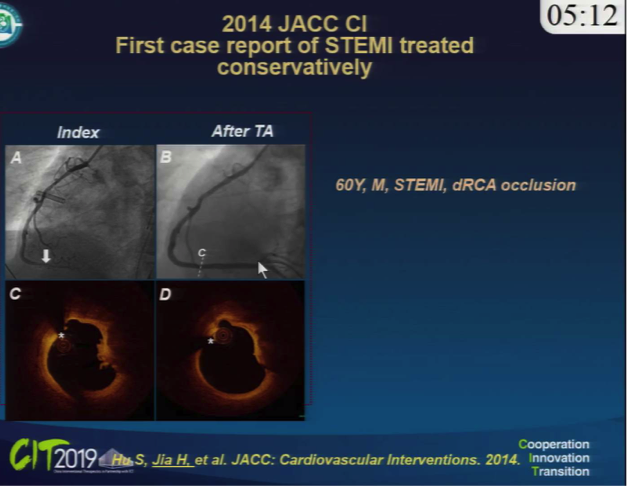
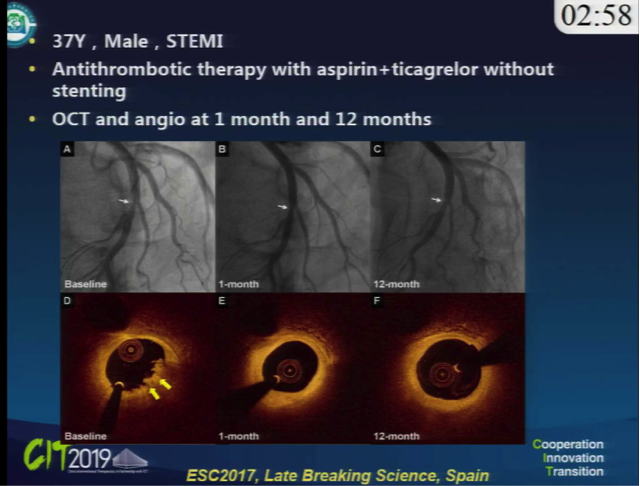
37岁,前降支中段闭塞,少量腹壁血栓,近端远端没有大的脂质斑块。抗血栓治疗1个月和1年后的结果对比。
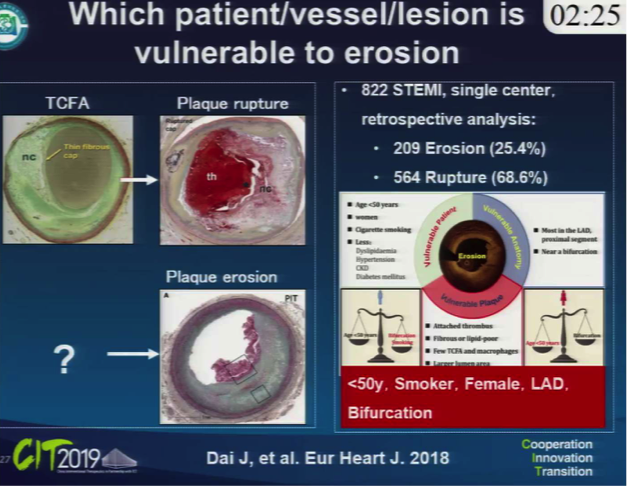
到底哪些患者和哪些病例容易出现斑块侵蚀?
小于50岁、吸烟(尤其女性)患者,在前降支的近端分叉位置更容易出现斑块侵蚀。
这一现象的机制目前尚不明确。
在抗栓药物治疗下,斑块侵蚀的愈合相对而言比斑块破裂愈合更好。
52岁男患者,溶栓后左冠状况良好,右冠有残余的白色血栓,无法判断是否破裂,近端有大脂质斑块。抗栓1个月后右冠状况良好,血栓完全降解,可见斑块破裂破口。

不破裂的斑块非常动态复杂,难以预测,可能会愈合,可能会进展,可能反复破裂愈合。

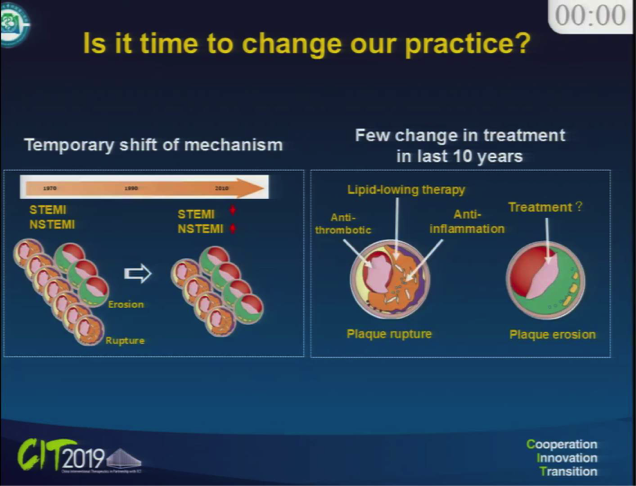
STEMI发生率逐渐下降,NSTEMI发生率逐渐增多。对破裂斑块,传统疗法抗栓、降脂、抗炎。但对非破裂斑块,还需进一步研究。
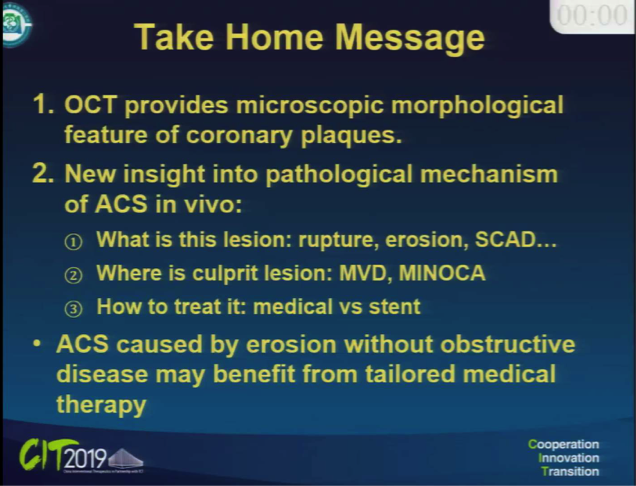
OCT对ACS患者非常有优势,包括血栓病变的判断、罪犯病变的识别,给支架治疗后的治疗策略提供信息。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CIT#
27
#介入心脏病学#
24
#于波#
32
#心脏病学#
23
#新发现#
24
#ST段抬高#
28
#ST段#
20
不错的,学习了,谢谢啦!
71