年终盘点:2017年JAMA杂志重磅级突破性研究成果
2017-12-15 MedSci MedSci原创
转眼间2017就要过去了,迎接我们的将是崭新的2018年,2017年医学顶尖杂志JAMA依然刊登了很多重磅级的研究,本文中小编就盘点了2017年JAMA杂志发表的一些非常有意义的亮点研究,与各位一起学习! 【1】中国城乡糖尿病患病率及死亡率 http://www.medsci.cn/article/show_article.do?id=5d288e8138e DOI:10.100
转眼间2017就要过去了,迎接我们的将是崭新的2018年,2017年医学顶尖杂志JAMA依然刊登了很多重磅级的研究,本文中小编就盘点了2017年JAMA杂志发表的一些非常有意义的亮点研究,与各位一起学习!
【1】中国城乡糖尿病患病率及死亡率
https://www.medsci.cn/article/show_article.do?id=5d288e8138e
DOI:10.1001/jama.2016.19720
近几十年来,中国糖尿病患病率大幅增加,但是目前还缺乏糖尿病相关的超额死亡率的可靠数据。2017年1月17日,JAMA刊登了中国慢性病前瞻性研究(China Kadoorie Biobank, CKB)项目的一项研究进展,公布了中国城乡糖尿病患病率及死亡率的数据。这是一项持续7年的全国前瞻性研究,涉及中国的10个地区(5个农村+5个城市),在2004年6月到2008年7月,共纳入30-79岁的512869名成年人,随访至2014年1月。
调查结果发现,5.9%的人患有糖尿病。农村地区的糖尿病患病率低于城市地区为,男性低于女性。随访364万人年,发现与无糖尿病人群相比,糖尿病患者的全死因死亡率显著增加,农村地区要高于城市地区。此外,该研究还发现,中国成年人中,糖尿病与很多心血管和非心血管疾病死亡率增加具有相关性。
正如文中结果所示,虽然城市地区的糖尿病患病率更高,但是农村地区糖尿病的超额死亡率更大。

【2】他汀一级预防应遵循哪个指南:USPSTF 还是ACC/AHA?
https://www.medsci.cn/article/show_article.do?id=4ab799e5502
DOI:10.1001/jama.2017.3416
他汀一级预防疗法相关指南推荐存在重要差异。美国预防服务工作组(USPSTF)强调疗法基于1个或多个心血管疾病(CVD)风险因素以及10年全球CVD风险为10%或以上。2017年4月,发表在《JAMA》的一项研究调查了美国成人中,假定完全应用USPSTF推荐,与美国心脏病学会/美国心脏协会(ACC/AHA)指南相比,他汀一级预防治疗的适应证差异。
研究使用2009~2014年年国家健康与营养调查(NHANES)数据,在3416例年龄在40至75岁、有空腹血脂数据、甘油三酯水平为400 mg/dL或更低,无既往CVD的具有全国代表性的样本中,评价遵循USPSTF 2016推荐vs ACC/AHA 2013胆固醇 指南,他汀治疗的适应证。
结果表明,与依从于ACC/AHA 2013指南相比,依从于USPSTF 2016关于他汀治疗的推荐导致更少的个体被推荐使用他汀作为一级预防,包括许多平均长期CVD风险较高的较年轻的患者。
【3】中国针灸研究首登国际顶级期刊JAMA,可有效减少女性压力性尿失禁患者的漏尿量
https://www.medsci.cn/article/show_article.do?id=0ffb103e61b9
DOI:10.1001/jama.2017.7220
继上次"电针治疗严重便秘"发表在国际名刊之后,中国中医科学院广安门医院刘志顺主任团队和中国中医科学院刘保延首席研究员团队携新研究再度来袭。
新的一项研究为多中心、中央随机、假电针对照的临床研究,在中国国内12家单位内完成。从2013年10月8日到2015年5月15日,共纳入504例受试者,2015年12月完成所有病例收集,旨在评估电针减少女性压力性尿失禁患者漏尿量的有效性和安全性。电针组穴位选取为双侧中髎(BL33)、会阳(BL35);假电针组穴位选取为双侧中髎对照点、会阳对照点,原穴横向向外旁开20mm。
其结果表明,与假电针相比,电针治疗6周,可以减少女性压力性尿失禁患者的漏尿量。但是,对于电针的长期效应和作用机制仍需进一步的研究。

【4】心源性卒中早期利伐沙班vs华法林
https://www.medsci.cn/article/show_article.do?id=d0ca1193514e
DOI:10.1001/jamaneurol.2017.2161
在卒中早期阶段,房颤相关急性缺血性卒中的复发缺血性卒中和脑出血的风险很高,包括出血转化。因为增加症状性颅内出血的风险,不推荐使用肝素。然而,如果使用阿司匹林治疗,房颤相关缺血性卒中2周内发生复发性缺血性卒中的几率为5%。临床上卒中后最常用的抗栓药物是阿司匹林,几天后或1-2周后当颅内出血的风险下降后开始给予口服抗凝剂治疗。但是,对于急性缺血性卒中,何时何人选择何种药物进行口服抗凝药物治疗尚不清楚。
2017年10月来自韩国的Keun-Sik Hong等在JAMA Neurology上公布了Triple AXEL试验结果,目的是为了验证房颤相关急性缺血性卒中患者使用利伐沙班vs华法林预防卒中早期复发的安全性和有效性。
Triple AXEL研究是一项随机、多中心、开放标签、盲法终点的2期临床试验,最终183名受试者完成研究,研究结果表明,对于轻型房颤相关急性缺血性卒中患者,利伐沙班和华法林的安全性和有效性相仿。

【5】口服胰岛素到底能不能延缓糖尿病发生
https://www.medsci.cn/article/show_article.do?id=5f95121e659f
DOI:10.1001/jama.2017.17070
1930年就有研究人员想研发口服胰岛素,此后关于改变胰岛素剂型的研究不断出现,但非注射胰岛素的很多关键技术难题依然没有办法解决。近日,JAMA杂志发表的一项随机对照试验结果显示,在一小部分研究参与者中,即那些已经显示出早期的低量胰岛素分泌人群中,口服胰岛素确实起了作用,可以延缓糖尿病的发生。
对于该结果,研究人员认为,出现1型糖尿病延迟发病的人是1型糖尿病的高危人群,可能已经发生了1型糖尿病,这些人是最容易产生胰岛素依赖。目前,该研究团队已经在一个新的试验里测试较高剂量的口服胰岛素,以观察口服胰岛素是否能更长地延缓病情。
【6】迄今最大肿瘤胚系基因测序显示,超过55%携带癌症相关基因突变的患者可能被漏检
https://www.medsci.cn/article/show_article.do?id=cc0f112485aa
DOI:10.1001/jama.2017.11137
近日,纪念斯隆凯特琳癌症研究中心(MSK)的研究人员在《JAMA》杂志上刊登了重磅研究成果。他们采用独特的肿瘤检测技术MSK-IMPACT,对1040名晚期癌症患者的410个癌症相关基因进行了测序,还对包括ACMG标准和指南所推荐的癌症易感基因在内的76个癌症相关基因突变进行了胚系分析。
研究的结果颇令人震惊:研究人员确定了182名患者携带临床上可靶向治疗的胚系癌症相关基因突变,占所有患者的17.5%,但以往的研究中,检测的结果只有3%-12.6%!这意味着这种分析方法更全面,当前的癌症相关基因检测方法,低估了携带易感基因癌症患者的比例。更让研究人员吃惊的是,如果根据患者的表型、家族史和现行的临床指南,这182名患者中将会有101名患者(55.5%),不会被建议去做基因检测!
采用这种新的分析方法,扩大癌基因检测的范围,既可以给癌症患者提供更加精确有效的个性化治疗,又能够给患者亲属提供遗传咨询,可谓是一举两得,对癌症的防治来说,是一个重大的突破!
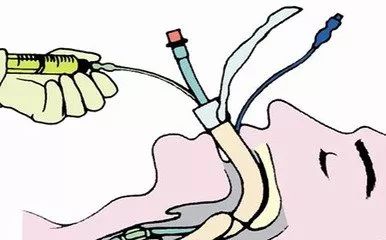
【7】长期机械通气镇静:右美托咪定优于咪达唑仑和丙泊酚
https://www.medsci.cn/article/show_article.do?id=18921088e7a6
DOI:10.1001/jama.2012.304
重症监护病房(ICU)的患者长期使用咪达唑仑或丙泊酚镇静会对患者产生严重的不良影响。右美托咪定是一种ICU镇静常用的α-2激动剂,可缩短机械通气时间,提高病人的舒适度。一项新的究探讨了右美托咪定与咪达唑仑或丙泊酚在维持镇静、缩短机械通气时间、改善患者护理舒适度方面的效果。
研究纳入2007-2010年间进行的3期多中心随机双盲临床 试验。其中MIDEX试验对比了咪达唑仑和右美托咪定在欧洲9个国家44个医疗中心ICU的使用情况;PRODEX试验比较了丙泊酚和右美托咪定在欧洲6个国家31个医疗中心和俄罗斯2个医疗中心的使用情况。
其结果表明,在接受长期机械通气的ICU患者中,右美托咪定维持患者轻中度镇静作用不低于咪达唑仑和丙泊酚。与咪达唑仑和丙泊酚相比,右美托咪定可以缩短机械通气的时间,改善了患者对疼痛的沟通能力。但是,右美托咪定发生不良反应相对更多。
【8】跨性别输血是否会升高死亡率
https://www.medsci.cn/article/show_article.do?id=a205116882d6
DOI:10.1001/jama.2017.15095
每当医务工作者遇到需要紧急输血的情况,他们会确保供血者和用血者血型相匹配,但没有人会关心供血者的性别。不过,最新的研究成果却对此提出了质疑。这项研究提出,接受了有怀孕史女性的血液后,小于50岁的男性用血者的死亡率更高。不过,这一结论及其背后的机理仍需进一步证实。
不过,参与这项研究的科学家和美国红十字会都认为,这项研究本身还不足以对目前的医疗工作产生实质性的影响,但如果这一发现在后续研究中得到进一步证实,就很有可能改变传统的输血匹配方式,这很可能延长全世界成千上万用血患者的生命。
目前,人们尚不清楚这一结论背后的生理学机制。科学家们推测,有怀孕史的女性的红细胞中,可能含有一些让年轻男性用血者产生更多排斥反应的免疫 因子。这一理论的主要观点是,曾生过男孩的女性可能具有一种抗体,它可以结合男性的Y染色体所产生的蛋白质,这可能是她们在孕期产生的一种正常免疫 反应。但新的研究无法验证该假说,因为研究者并不能获得女性供血者后代的性别数据。

【9】降压目标值存在争议
https://www.medsci.cn/article/show_article.do?id=7282884558a
DOI:10.1001/jama.2017.0105
美国高血压指南JNC 7公布几年后,普遍认为对于一般患者,血压应控制在140/90 mmHg以下而无论其年龄;对于合并糖尿病、慢性肾病和一些心血管疾病的患者,血压目标值应控制在130/80 mmHg以内。然而,随着ACCORD和SPRINT的结果的公布,对降压目标值提出了新的挑战,特别是对老年患者。
两个试验都是随机、对照、开放标签研究,旨在比较将患者SBP降低到低于140 mmHg(标准治疗)或120 mmHg(强化治疗)的影响。在ACCORD研究中,尽管强化治疗组脑卒中 率显著下降、心血管疾病(CVD)出现无统计学意义的减少,但是在主要终点方面与标准化治疗组无显著差异。SPRINT研究结果显示,较标准治疗而言强化治疗显示了显著的获益。另一个重要发现是对于75岁以上患者来说,获益程度与年轻人群持平。
降压的最终目标是预防高血压的发生,对于高血压早期的人来说,特别是血压水平在130-139/85-89 mmHg范围内的患者,应强调通过健康的生活方式来控制血压。此外,对所有高血压患者来说,都应考虑使用他汀类药物并且努力戒烟,以减少心血管并发症的发生。

【10】急性缺血性卒中和大血管闭塞治疗——接触穿刺vs摘取支架
https://www.medsci.cn/article/show_article.do?id=283510e48131
DOI:10.1001/jama.2017.9644
接触穿刺与摘取支架是治疗缺血性卒中和大血管闭塞的一线疗法,但是孰优孰劣仍不清楚。近日,一项新的临床试验研究考察了不同的中风后血管重建方法对急性缺血性脑卒中患者的影响。ASTER研究是一项随机、开放标签、盲终点的临床试验,在法国的8个综合卒中中心开展,对比了接触穿刺技术与标准血栓摘取支架对急性缺血性卒中和大血管闭塞患者血管重建的效果以及不良事件。
结果显示,两组患者血管重建的成功概率相当,临床受益与严重术后不良事件也无显著差异。因此,研究认为,对接受手术前的循环缺血性卒中患者,接触穿刺与血栓摘取支架在血管重建成功率、预后以及不良事件方面不存在显著差异。

【11】乔杰院士和洪天配教授共同领导的随机对照临床试验POSTAL研究结果在JAMA发表
https://www.medsci.cn/article/show_article.do?id=80ff12336275
doi:10.1001/jama.2017.18249
2017年12月12日,JAMA(IF=44.405)正式发表了北京大学第三医院(北医三院)内分泌科、生殖医学中心、临床流行病学研究中心等组成的跨学科研究团队合作完成的随机对照临床试验(RCT)的研究结果。这项RCT研究的名称为:甲状腺功能正常的甲状腺自身免疫状态妇女接受左旋甲状腺素治疗后的妊娠结局研究(Pregnancy Outcome Study in enthyroid women with Thyroid Autoimmunity after Levothyroxine,简称POSTAL研究)。
该研究是甲状腺自身免疫状态与体外受精-胚胎移植(IVF-ET)妊娠结局相关研究领域迄今为止国际上报道的临床研究中样本量最大的RCT研究。
该研究采用RCT的研究设计和方法,从30000多例不孕症妇女中进行筛选,并最终入组600例TPOAb阳性但甲状腺功能正常的不孕症妇女,随机分为干预组和对照组各300例。两组患者均采用标准的IVF-ET操作流程,并按照相同的随访方案进行现场随访和电话随访,以监测并记录随机分组的依从性和妊娠结局。动态监测孕期甲状腺功能的变化,以指导左旋甲状腺素的剂量调整。
POSTAL研究结果表明,左旋甲状腺素治疗并不能改善TPOAb阳性但甲状腺功能正常的不孕症妇女的IVF-ET妊娠结局,干预组和对照组的流产率分别为10.3%和10.6%,临床妊娠率分别为35.7%和37.7%,活产率分别为31.7%和32.3%,两组间均未见显着差异。
本研究结果提示,甲状腺功能正常但甲状腺自身抗体阳性的不孕症女性在进行IVF-ET过程中不需要预防性应用左旋甲状腺素,但需要监测甲状腺功能的变化。
值得注意的是,由于本研究排除了具有反复流产史的患者,故本研究结论对于流产高风险的不孕症患者可能并不适用。
以上研究仅是小编整理的一些重大突破性研究,当然2017年还有很多很多值得我们去认真学习和钻研的亮点研究,相信在即将到来的2018年JAMA杂志上将会为我们呈现出更多创新性的突破研究,让我们拭目以待。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JAMA杂志#
37
#研究成果#
31
#突破性研究#
31
#年终盘点#
34
#重磅#
33
学习
70
学习学习.了解了解
63
学习了新知识
67