Alzheimers Dementia: 调查400万人,痴呆的患者何临床特征?
2022-03-27 网络 网络
痴呆症存在着相当大的差异,这为预防和提供病人护理的优先事项提供了参考
 老年痴呆症是全世界老年人口中死亡和发病的一个主要原因。在英国,自2011年以来,痴呆症是女性最常见的死亡原因,自2015年以来是男性的第二大死亡原因。
老年痴呆症是全世界老年人口中死亡和发病的一个主要原因。在英国,自2011年以来,痴呆症是女性最常见的死亡原因,自2015年以来是男性的第二大死亡原因。
患有痴呆症的人很可能有合并症,除了与痴呆症相关的疾病外,还需要更多的保健关注。因此,痴呆症和多种长期病症都可能给患者的健康、医疗服务的使用和社会护理服务带来巨大负担。
痴呆症的定义是认知功能的下降,足以影响日常生活活动或社会功能。阿尔茨海默病(AD)和血管性痴呆是比较常见的痴呆类型,如果有关于痴呆亚型的信息的话。
了解人口层面的痴呆症发病率、死亡率、相关疾病,以及患者如何在医疗系统中就诊和进展,对于计划和制定在疾病发展的特定阶段可能有价值的干预措施以支持个人和减少痴呆症的社会负担是必要的。
目前还缺乏对痴呆症患者如何、何时以及为何进入医疗系统的详细了解。虽然以前的痴呆症研究提供了对疾病负担的见解,但它们的范围有限,因为关于区域队列或调查的报告无法提供对痴呆症合并症和医疗资源使用的精确估计。
藉此, 英国UCL的Sheng-Chia Chung通过使用常规收集的初级电子健康记录(EHR)数据,与英国430万个人的二级护理和死亡数据相联系,克服了这一局限性。
他们调查了发病率、合并症、临床就诊原因、死亡率和死亡原因。研究了包括性别和贫困在内的亚组的疾病模式。这些开始提供了对卫生保健系统中记录的痴呆症进展的洞察力,以指导沿着疾病路径的有针对性的干预措施。
他们对英国430万人的联网电子健康记录进行了纵向队列分析,以调查痴呆症的发病率和死亡率。对有和没有痴呆症的人的住院原因和死亡原因进行了比较。
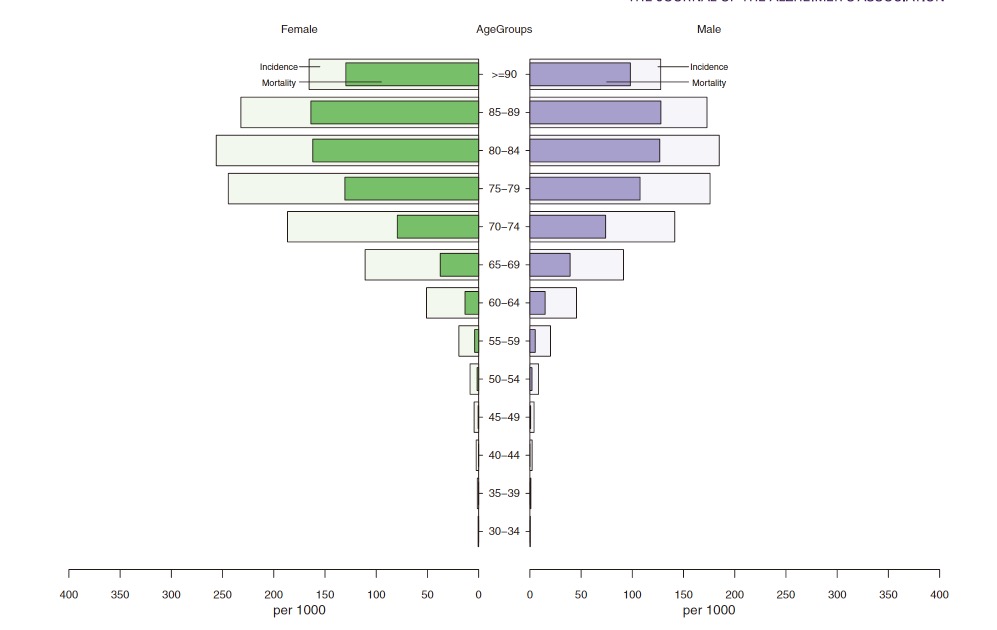
从1998年到2016年,他们观察到145,319人(3.1%)患有事件性痴呆症。
在痴呆症诊断之前,观察到老年人因感染、未知的发病率而反复住院,以及因慢性疼痛而多次去初级保健。
有一半的人在诊断时存在多种长期疾病。生活在高贫困地区的个体有较高的痴呆症发病率和高死亡率。
该研究的重要意义在于发现了:痴呆症存在着相当大的差异,这为预防和提供病人护理的优先事项提供了参考。
原文出处:
Chung S, Providencia R, Sofat R, et al. Incidence, morbidity, mortality and disparities in dementia: A population linked electronic health records study of 4.3 million individuals. Alzheimer’s & Dementia. Published online March 15, 2022:alz.12635. doi:10.1002/alz.12635
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#ERS#
32
#alzheimers#
42
#dementia#
48
#临床特征#
37
#MERS#
46
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
27