Sci Transl Med:4天将皮肤细胞变成专杀脑癌细胞的「干细胞杀手」
2017-02-05 节后开工的奇点糕 奇点网
《科学 转化医学》封面 想象一下,有一种细胞可以在脑癌患者的脑中“穿梭”,捕捉癌细胞并且消灭它们,在完成“使命”后,悄悄消失,是不是很神奇呢?可谓是“事了拂衣去,深藏功与名”。这种颇具侠客精神的细胞的“真实身份”就是神经干细胞,它真的有这么厉害吗? 2月1日,北卡罗来纳大学教堂山分校的Shawn Hingtgen教授将他们的研究成果作为封面文章发表在了《科学 转
《科学 转化医学》封面
想象一下,有一种细胞可以在脑癌患者的脑中“穿梭”,捕捉癌细胞并且消灭它们,在完成“使命”后,悄悄消失,是不是很神奇呢?可谓是“事了拂衣去,深藏功与名”。这种颇具侠客精神的细胞的“真实身份”就是神经干细胞,它真的有这么厉害吗?
2月1日,北卡罗来纳大学教堂山分校的Shawn Hingtgen教授将他们的研究成果作为封面文章发表在了《科学 转化医学》杂志上。他们利用细胞重编程技术,将人的皮肤细胞转分化为诱导性神经干细胞(iNSCs),利用它携带药物,这种治疗方法让胶质母细胞瘤小鼠脑内的肿瘤缩小到原来的2-5%,显著延长了小鼠的生存时间!

Shawn Hingtgen教授
包括脑瘤在内的一些癌症,它们会产生化学信号,吸引干细胞靠近。我们知道,干细胞的再生功能能够帮助修复受损细胞和组织,有科学家认为,干细胞可能会在信号的诱导下,将肿瘤识别成受损需要愈合的伤口,利用了这一点,使得干细胞分化出癌细胞,继而扩散。于是就有研究人员受此启发,想能不能让干细胞作为“卧底”,深入普通药物不能进入的“细枝末节”处,杀死癌细胞,阻止扩散呢?
Hingtgen教授也想到了这一点,他在众多候选中选择了神经干细胞,神经干细胞是专能干细胞,只能分化成各类神经细胞,因此不用担心它们被癌细胞“拐跑”,分化为癌细胞。在一年前的研究中,Hingtgen教授用成纤维细胞重编程得到了iNSCs,并且证实了它们可以移动至大脑任意一处,“追踪”癌细胞。此外,他们还发现,对iNSCs进行了基因工程改造后,除了“追踪”的本领,它们还获得了产生一种诱导癌细胞凋亡的因子的能力,这种因子叫做TRAIL。用iNSCs治疗的胶质母细胞瘤小鼠的生存率提高了160-220%!这些成果发表在了2016年2月的《自然通讯》杂志上[2]。

重编程得到的人源神经干细胞
不到一年的时间里,Hingtgen教授带领他的团队又取得了新的进步。他们不仅用人的皮肤细胞成功得到了iNSCs,而且只需要4天的时间就可以做到。Hingtgen教授说:“‘速度’是至关重要的,过去我们需要几个星期的时间才能将人类的皮肤细胞转化为干细胞,但是脑癌患者没有那么多时间可以等,所以我们开发出了新方法,足够快,也足够简单,让患者可以很快就用上。”
传统的诱导成熟细胞重编程成为干细胞要用到四种因子:Oct4、Sox2、Klf4、c-Myc,也就是“山中因子”,这是当年山中伸弥教授的研究成果。而Hingtgen教授只用到了其中的一个——Sox2,在实验中,将人的皮肤细胞与Sox2因子共同培养,研究人员观察到,到48小时,细胞形态就开始发生变化,逐渐形成神经干细胞和神经球(神经干细胞在体外扩增培养的表现形式)。经过追踪,研究人员发现,直到第10天,细胞依然稳定的保持在神经干细胞状态不发生改变。
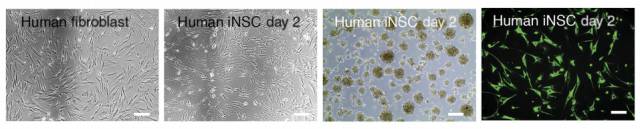
从左至右依次为: 人的成纤维细胞(皮肤细胞是其中一种)、2天后开始产生的神经干细胞、神经球、荧光染色的神经干细胞
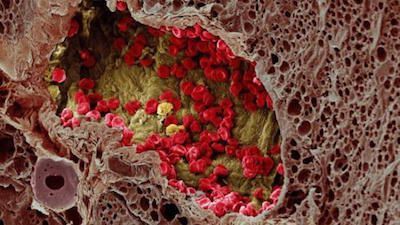
对得到的iNSCs进行基因工程改造后得到了可以产生TRAIL因子的干细胞(h-iNSCTE–sTR),用这些干细胞,研究人员对移植了人的胶质母细胞瘤的小鼠进行了注射。他们发现,未接受治疗的小鼠存活天数平均为25天,而接受了治疗的小鼠则为51天,它们的存活天数增加了50%!而且,研究人员观察到,接受了治疗的小鼠的肿瘤缩小到了未接受治疗小鼠的1/50-1/20不等!
有了这个鼓舞人心的结果,研究人员又琢磨,如果让干细胞荷载药物,会不会比产生TRAIL因子的治疗效果好呢?小鼠会不会活得更久呢?于是他们选择了一种前体药物(前体药物是经过化学修饰后得到的,在体外没有生物活性或活性很低,在体内随着代谢,经过酶的催化等才能释放出活性药物,发挥药效。前体药物增加了药物的生物利用度和靶向性,降低了药物的毒副作用。)进行了实验,在治疗结束后,接受治疗的小鼠的平均存活天数达到了67天 !这一结果显然超过了TRAIL因子的效力。

I为对照组,J为接受荷载着前体药物的干细胞注射的脑内荧光染色图,绿色荧光为胶质母细胞瘤
最后,研究人员们模拟了临床上的治疗过程,先对小鼠进行了肿瘤切除,然后再注射荷载了前体药物的干细胞。结果显示,接受了干细胞注射的小鼠肿瘤的复发速度减慢,复发瘤的大小相较未接受注射的小鼠小3.5倍,接受了注射的小鼠的最长生存期超过了70天。
对于这一系列的研究成果,来自维克森林再生医学研究所的癌症生物学家Frank Marini对《科学》杂志表示,尽管他没有参与这项研究,但是他认为这是一个“伟大的开始”,因为治疗开始很快,效率也相对较高。同时Marini指出,后续还需要研究人员对干细胞究竟能延伸多远进行严格的测试。Hingtgen教授也表示,他们计划在一到两年内进入临床实验,使用患者自身的皮肤细胞,尽量避免免疫排斥问题,以及对干细胞注射量的有效性和安全性进行评估。
这是首次,研究人员将人类的干细胞与脑癌治疗联系到一起,Hingtgen教授认为,“我们在将它变为真正的治疗方法的路上已经迈近了一大步,这会为脑癌的治疗带来不小的改变。”
原始出处:
Bagó JR, Okolie O, Dumitru R, Ewend MG, Parker JS, Werff RV, Underhill TM, Schmid RS, Miller CR,Hingtgen SD. Tumor-homing cytotoxic human induced neural stem cells for cancer therapy. Sci Transl Med. 2017 Feb 1;9(375). pii: eaah6510. doi: 10.1126/scitranslmed.aah6510.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Transl#
34
#TRA#
34
好东西大家一起学!
67
新进展,值得学习
73
#癌细胞#
34
#脑癌#
34
#皮肤细胞#
30
#Med#
22
如果临床应用的话,会给患者带来希望的。渴望推广,好文点赞了!
74
好厉害,加油
66