Circulation:特发性扩张型心肌细胞中存在的永久性病毒基因组
2019-05-18 MedSci MedSci原创
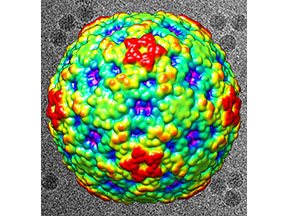
B组肠病毒是急性心肌炎的常见病因,也是慢性心肌炎和扩张型心肌病的先兆,还是心脏移植的首要原因。目前,在扩张型心肌病的发展过程中所涉及的特定的病毒功能尚不明确。从扩张型心肌病患者心肌组织的RNA中鉴定肠病毒RNA 5’端序列。经二代RNA测序,体外构建模拟在人类样本中发现的肠病毒RNA序列的病毒cDNA克隆,并在培养的原代人心肌细胞中评估其复制和对宿主细胞功能的影响。主要鉴定出以5'端基因组RNA缺
从扩张型心肌病患者心肌组织的RNA中鉴定肠病毒RNA 5’端序列。经二代RNA测序,体外构建模拟在人类样本中发现的肠病毒RNA序列的病毒cDNA克隆,并在培养的原代人心肌细胞中评估其复制和对宿主细胞功能的影响。
主要鉴定出以5'端基因组RNA缺失(17-50个核苷酸)为特征的B组肠病毒,偶有混杂低比例的具有完整5'端基因组的病毒。原位杂交和免疫组织学实验在心肌细胞中检测到这些永久性的基因组。向原代人心肌细胞转染病毒RNA发现,在没有检测到病毒斑块形成的情况下,部分缺失的基因组RNAs表现出早期复制活性,而缺失和完整RNA的混合形式可产生能诱导细胞病变的微粒,诱导病变的效应不同于单纯全长RNA的诱导效应。此外,在人类心肌细胞中,缺失或全长和混合的病毒RNA能够指导翻译和产生具有蛋白水解活性的病毒蛋白酶2A。
本研究表明,在不明原因的扩张型心肌病中,持续存在的病毒主要是基因组RNAs 5'端存在片段缺失,伴或不伴有携带全长辅助RNAs的B组肠病毒,可通过合成具有蛋白水解酶活性的病毒蛋白酶2A损伤心肌功能。本研究结果有助于我们更好的理解EV在人类心肌组织中持续存在的分子机制,并促进基于B组柯萨奇病毒蛋白酶2A活性的特异性抑制剂的用于急性/慢性心肌感染的新型治疗策略的发展。
Alexis Bouin , et al.Enterovirus Persistence in Cardiac Cells of Patients With Idiopathic Dilated Cardiomyopathy Is Linked to 5’ Terminal Genomic RNA-Deleted Viral Populations With Viral-Encoded Proteinase Activities. Circulation.14 May 2019. https://doi.org/10.1161/CIRCULATIONAHA.118.035966. 2019;139:2326–2338
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#扩张#
23
#特发性#
32
学习学习
66
谢谢分享学习
75
有用
58