Lancet:IL-17A/F纳米体索洛奇单抗治疗斑块型银屑病II期临床获得成功
2021-04-26 MedSci原创 MedSci原创
索洛奇单抗30-120mg剂量均表现出良好的中重度斑块型银屑病治疗效果,其具有起效快速,改善持久,以及较好安全性的特点
白细胞介素-17家族包含6个亚型,其中。IL-17A和IL-17F与银屑病的发病相关,二者可以构成同型或异质二聚体并通过白细胞介素-17RA/RC受体复合体发出信号。目前已有多个IL-17单克隆抗体用于银屑病的治疗。索洛奇单抗是一种新型三价纳米体,近日研究人员考察了索洛奇单抗对斑块型银屑病患者的疗效、安全性和耐受性。
研究组在保加利亚、加拿大、捷克、德国、匈牙利、波兰和美国的41个医疗机构开展,为多中心、随机、安慰剂对照、临床IIb期试验。年龄在18-75岁的,中重度斑块型银屑病患者参与研究,随机分为6组,分别为安慰剂组、30 mg索洛奇单抗组、60 mg索洛奇单抗组、索洛奇单抗120 mg正常负荷组、索洛奇单抗120 mg增强负荷组或苏金单抗300 mg组。所有参与者先接受4周的筛选治疗,随后是12周的对照诱导期,再之后是12周的剂量维持或升级治疗以及24周的反应评估或剂量保持治疗。研究的主要终点为12周时IGA得分0-1的患者比例(皮肤病变完全清除或几乎清除)。
313名患者参与研究,其中安慰剂组52人、索洛奇单抗30 mg组52人、索洛奇单抗60 mg组52人、索洛奇单抗120 mg正常负荷组53人、索洛奇单抗120 mg增强负荷组51人、苏金单抗300 mg组53人。各组参与者的基线特征相似。12周时,各组主要终点达标情况如下:安慰剂组0人(0%)、索洛奇单抗30mg组25人(48.1%)、索洛奇单抗60mg组44人(84.6%)、索洛奇单抗120mg正常负荷组41人(77.4%)、索洛奇单抗120mg增强负荷组45人(88.2%),苏金单抗组41人(77.4%)。研究期间,索洛奇单抗组最常见的不良事件包括鼻咽炎(13.5%)、瘙痒(6.7%)和上呼吸道感染(4.3%)。1名索洛奇单抗组患者发生克罗恩病。研究期间,索洛奇单抗表现出的安全性与苏金单抗相似,但念珠菌感染风险较高(17.4% vs 1.9%)。
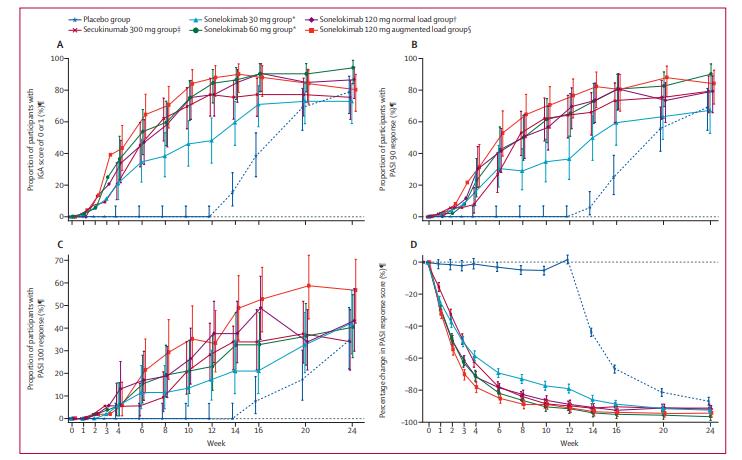
研究认为,索洛奇单抗30-120mg剂量均表现出良好的中重度斑块型银屑病治疗效果,其具有起效快速,改善持久,以及较好安全性的特点。
原始出处:
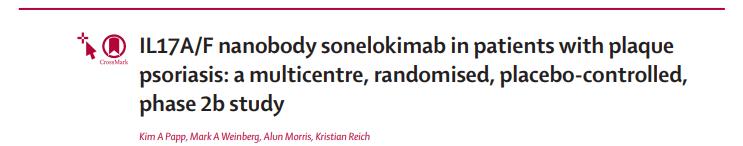
Kim A Papp et al. IL17A/F nanobody sonelokimab in patients with plaque psoriasis: a multicentre, randomised, placebo-controlled, phase 2b study.Lancet. April 24, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
35
#I期临床#
27
#斑块#
30
#IL-17#
52
#IL-17A#
39
#斑块型银屑病#
45
#IL-1#
34
#II期临床#
27
不错
60
顶刊就是不一样,质量很高,内容精彩!学到很多
53