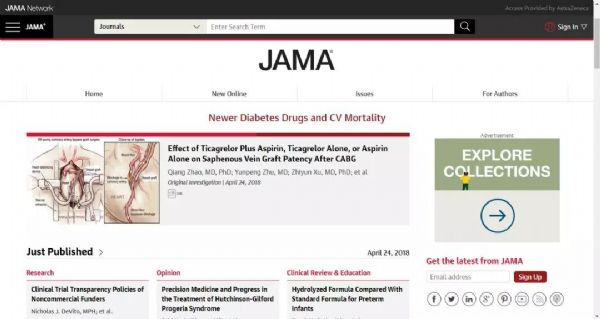
重磅:“心-桥”研究:上海交通大学瑞金医院牵头的原创性RCT研究发表于JAMA
2018-04-26 MedSci MedSci原创
这一重大临床问题由上海交通大学医学院附属瑞金医院心脏外科的赵强教授团队首次通过RCT研究— DACAB取得了突破性的解答。
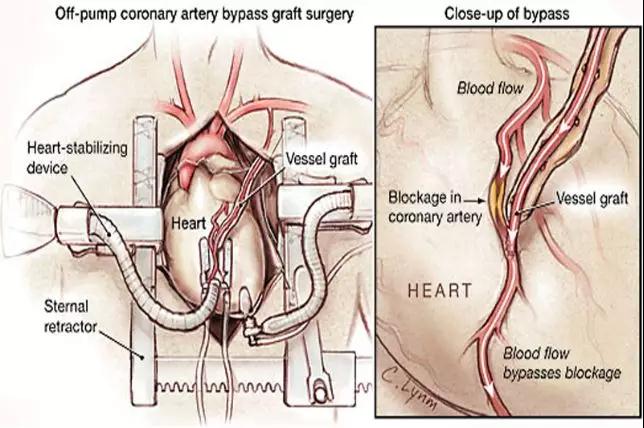
▍研究背景
根据循证指南,冠脉动脉旁路移植术(CABG)依然是冠心病左主干或多支病变的“金标准”血运重建方式,尤其对于合并糖尿病或左室功能不全的患者。桥血管的通畅是CABG术中后远期疗效的根本保证。与冠脉支架类似,抗血小板治疗是保障桥血管的通畅的药物治疗基石。在现有经典的阿司匹林单抗循证实践基础上,如何进一步提高桥血管的通畅率?这一重大临床问题由上海交通大学医学院附属瑞金医院心脏外科的赵强教授团队首次通过RCT研究— DACAB取得了突破性的解答。近日该研究正式发表于全球“医学四大刊”之一的《美国医学会杂志(JAMA)》(五年影响因子为44.405)并成为本周JAMA主页头条。
▍研究方法
DACAB研究是一项前瞻性、随机、开放标签、平行对照的多中心临床研究(NCT02201771),旨在比较替格瑞洛与阿司匹林联用(T+A组)、单用替格瑞洛(T组)或单用阿司匹林(A组)患者的术后一年SVG通畅率。该研究假设包括两个独立的有效性检验:T+A组与A组的比较,T组与A组的比较。
纳入标准为18~80岁的单纯择期CABG患者。关键排除标准包括:血流动力学不稳定;临床指证必须术后DAPT或口服抗凝治疗;已知严重出血风险;已知有研究药物相关禁忌证。
经过统计学样本量估算,研究筛选了2014.8-2015.11国内六家大学附属医院的1256例CABG患者,最终连续随机了500例受试者(1460 SVG桥血管样本)。受试者以1:1:1的比例随机分为3组:替格瑞洛90mg Bid + 阿司匹林100mg Qd(T+A组,n=168),替格瑞洛90mg Bid(T组,n=166),阿司匹林100mg Qd(A组,n=166),并于CABG术后24小时内开始接受随机分配的抗血小板治疗方案直至术后12月。采用多层螺旋CT血管造影(MSCTA)或冠脉造影(CAG) 技术,以Fitzgibbon 标准,并最终由独立的影像数据评审中心(IDRC )评价桥血管结局。(图1)
研究同时随访记录了受试者的MACE和出血事件等关键临床结果。
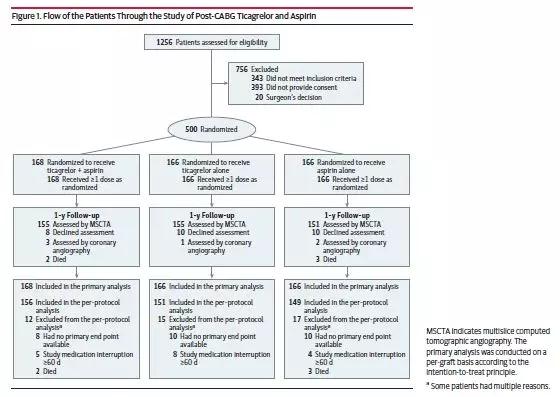
图1. 临床试验分组与流程
▍研究结果
最终所有500例受试者均完成了临床随访,其中467例(93.4%)受试者接受了12个月时的CCTA/CAG桥血管影像学检查并得到了首要终点SVG结局数据(1369/1460,93.8%)。研究首要终点SVG通畅率比较严格采用意向性分析原则(ITT),无法获得结局数据的SVG(6.2%)一律按不通畅/闭塞统计。ITT分析结果:T+A组SVG通畅率(Fitzgibbon A级)为88.7% (432/487),T组为82.8%(371/485),A组为76.5% (404/488)。T+A组较A组高12.2%(95% CI 5.2-19.2%,P=0.0006),达到了研究假设的统计学差异。T组比A组高6.3% (95% CI -1.1-13.7%,P=0.0962),有趋势但尚未达到研究假设的统计学差异。
次要临床终点方面,1年MACE事件发生率:T+A治疗组为3例(1.8%);T治疗组为4例 (2.4%);A治疗组为9例(5.4%)。TIMI定义的大出血事件,三组发生率均较低(T+A组 3例,T组2例,A组 0);其中CABG相关的出血T+A组 1例,T组1例,A组未发生。而非CABG相关的出血事件总体发生率T+A组较高,主要分布在轻微出血。

表1. 替格瑞洛联合阿司匹林双抗 vs 阿司匹林单抗;替格瑞洛单抗 vs 阿司匹林单抗的主要终点结果分析
▍研究总结
对于DACAB研究1年结果,主要研究者、文章第一兼通讯作者赵强教授总结道:与阿司匹林单药治疗相比,替格瑞洛联合阿司匹林的双联抗血小板治疗方案可显著提高CABG术后1年的静脉桥血管通畅率,同时存在减少MACE的趋势。
另据共同第一作者朱云鹏医生介绍,抗血小板治疗对于CABG术后的治疗获益应该远不局限于桥血管通畅,更在于临床事件(死亡、心梗、脑梗、再次血运重建等)的获益。由于CABG的独特之处,桥血管病变与临床MACE的关联不像支架再狭窄与临床MACE的关联那么强烈而明确。故随刊发表的国外权威学者评论也指出,期待DACAB研究的长期随访结果和世界范围内更多的同领域临床研究的开展,进一步证实强化抗血小板治疗对CABG术后临床终点疗效的获益。
▍梅斯点评
CABG术后远期通畅率,一直是临床关心的问题,术后积极抗血小板治疗,被认为是其中重要的策略。但是,研究认为一年 术后SVG闭塞率在15-20%,这些患者往往容易再发心梗,甚至死亡。因此,如何进一步降低桥血管闭塞,也成为新的热点。2013年一项meta分析发现,氯吡格雷联合阿司匹林,能更好降低桥血管闭塞率。目前多项指南都推荐双抗作为降低CABG术后桥血管闭塞率的重要的方案,但是缺乏大样本、高级别推荐证据。同时,过去还有部分研究结果存在争议,如早期的 CASCADE研究发现阿司匹林联合氯吡格雷与单纯阿司匹林相比,并没有观察到抑制大隐静脉血管桥(SVG)的内膜增生。这很有可能与研究人群的风险度相对较低,阿司匹林本身就已能提供足够的保护。那么,在更高的风险人群中,如何有效达到保护作用?另外,PLATO-CABG亚组结果提示替格瑞洛显著降低CABG术后死亡风险和心血管死亡风险,那么,替格瑞洛降低CABG术后的死亡风险主要获益原因是否与桥血管闭塞率下降有关呢?这篇研究正好回答这个问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#重磅#
39
#交通#
31
腻害
79
不错耶.学习了
82
已学习
80
学习学习学习
76