BMJ:除了下肢血管彩超,小小D二聚体也能提示深静脉血栓形成!
2022-02-19 MedSci原创 MedSci原创
使用临床试验前概率和D-二聚体相结合的诊断策略在随访期间确定了一组低风险的深静脉血栓患者,同时大大减少了对超声成像的需求。
临床评估、D-二聚体(DD2)血液检测和超声成像被广泛用于评估可疑的下肢深静脉血栓(DVT)。有证据表明,三项评估中任何两项的出现,即临床预检概率低、DD2检测阴性(<500 ng /mL)、近端静脉超声成像阴性,都与随后发生血栓性并发症的概率极低有关,可以排除深静脉血栓。
为了评价DVT诊断算法的安全性和效率,来自加拿大麦克马斯特大学医学系的专家开展了一项前瞻性诊断管理研究。将来自加拿大的大学急诊部或门诊部的有深静脉血栓症状或体征的患者进行检测,结果发表在BMJ杂志上。
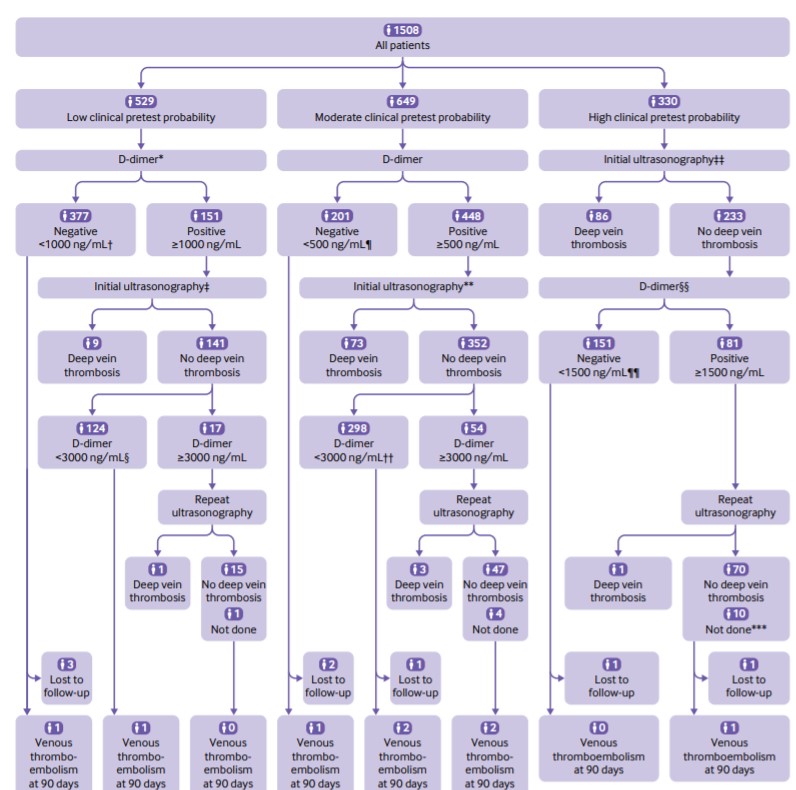
该研究假设在Wells低临床预检概率和DD2<1000 ng/mL或Wells中度临床预检概率和DD2<500 ng/mL的情况下被认为可以排除DVT,而无需进一步检查。所有其他患者都有近端超声成像。重复近端超声造影仅限于最初超声造影阴性、低度或中度临床预检概率和DD2 >3000 ng/ml或高度临床预检概率和DD2>1500 ng/ml的患者。如果没有诊断出深静脉血栓,患者不接受抗凝血治疗。主要结果是三个月后出现无症状的DVT。
结果显示,1508名患者被纳入并进行了分析,其中173人(11.5%)在预定的诊断测试中患有DVT。在1275名在预定检测中没有近端DVT且没有接受抗凝治疗的患者中,有8人(0.6%,95%置信区间为0.3%至1.2%)在随访中被发现有DVT。
与传统的深静脉血栓检测策略相比,这种诊断方法将超声检查的需求从平均1.36次/病人减少到0.72次/病人(差异为-0.64,95%置信区间为-0.68至-0.60),相当于相对减少47%。
综上,使用临床试验前概率和D-二聚体相结合的诊断策略在随访期间确定了一组低风险的深静脉血栓患者,同时大大减少了对超声成像的需求。
参考文献:
Diagnosis of deep vein thrombosis with D-dimer adjusted to clinical probability: prospective diagnostic management study. BMJ 2022; 376 doi: https://doi.org/10.1136/bmj-2021-067378
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#静脉#
38
#静脉血#
43
#二聚体#
34
#BMJ#
35
#静脉血栓形成#
41