JAMA Psychiatry:当心!冠心病患者可能得了“双心病”!
2021-08-21 MedSci原创 MedSci原创
艾司西酞普兰治疗焦虑对减少冠心病患者的焦虑是安全和有效的。
据世界心脏联盟估计,在全世界范围内25岁以上的成年人中,每3人就有1人将罹患心血管疾病,每年超过1720万人死于心血管疾病。与此相应,近年来我国的心血管疾病发病率和死亡率持续攀升,而焦虑、抑郁是心血管病患者常见的并发症。
当今生活节奏越来越快,竞争日益激烈,与之而来的是人们生活工作压力也越来越大。不少人在高强度负荷下得不到有效的缓解,出现了相应程度的心理问题,严重的甚至会患上精神性疾病,如焦虑症、抑郁症等。
鲜为人知的是,这些心理疾病可能是心血管疾病的并发症。据报道,焦虑抑郁在冠心病患者中的发生率极高,约为18%~60%。焦虑抑郁状态和重症抑郁状态都会增加冠心病患者的并发症和死亡率,它也是冠心病生理进展中一个独立高危险因素。
遗憾的是,通常心内科医生往往不能识别患者的抑郁焦虑状态,从而不能有效地控制患者的病情。大约60%~70%的抑郁症患者,是以各种躯体症状作为主诉而就诊于各内科的专科或普通门诊中,而内科医生对其本质是心理障碍的识别能力仅约15%。
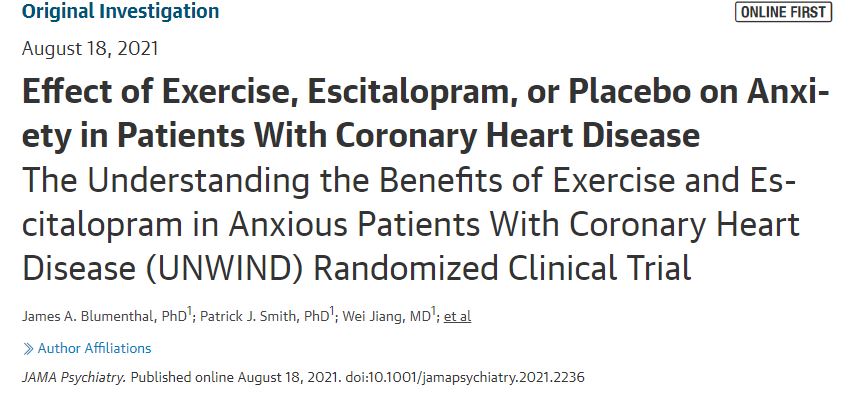
然而,对冠心病患者的焦虑的有效治疗还不确定。为了确定运动和艾司西酞普兰在减少由医院焦虑和抑郁-焦虑分量表(HADS-A)测量的焦虑症状以及改善冠心病风险生物标志物方面是否优于安慰剂,近期来自杜克大学医学中心精神病学和行为科学部的专家开展了相关研究,结果发表在JAMA Psychiatry杂志上。
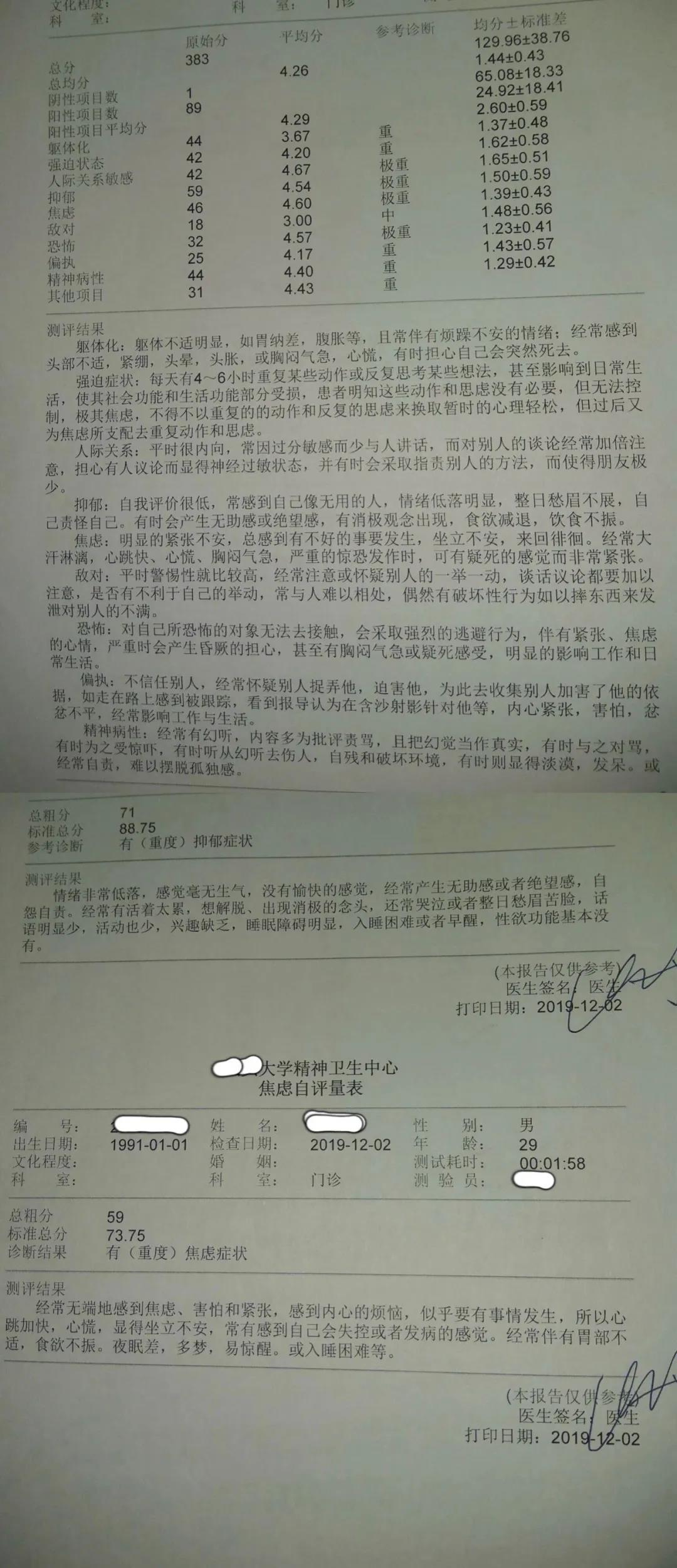
这项随机临床试验于2016年1月至2020年5月在美国一家三级护理教学医院进行,包括128名患有稳定的冠心病和被诊断为焦虑症或HADS-A≥8的门诊病人,他们年龄超过40岁,往往久坐,目前没有接受心理健康治疗。
干预措施为进行12周的有氧运动,每周3次,强度为70%至85%的心率储备,艾司西酞普兰(每天最多20mg),或相当于安慰剂的药物。该研究包括128名参与者。平均(SD)年龄为64.6(9.6)岁,37名参与者(29%)为女性。
结果显示,与随机接受安慰剂的人相比(-3.5;95% CI,-4.5~-2.4)运动组和艾司西酞普兰组的参与者报告了HADS-A减少更加明显(运动=-4.0;95%CI,-4.7~-3.2;艾司西酞普兰=-5.7;95%CI,-6.4~-5. 0)。与随机接受运动的人相比,随机接受艾司西酞普兰的人报告焦虑症状较轻(-1.67;95% CI,-2.68~-0.66;P =.002)。
三组参与者随访期间的HADS-A得分
同时,发现干预后24小时尿液中儿茶酚胺(提示焦虑相关的激素水平)的组间差异显著(运动z得分=0.05;艾司西酞普兰z得分=-0.24;安慰剂z得分=0.36)。与安慰剂组相比,运动组和艾司西酞普兰组的下降幅度更大(F1,127 = 4.93),与运动组相比,艾司西酞普兰组的下降幅度更大(F1,127 = 4.37)。但所有组别在CHD生物标志物方面都取得了相似但微小的变化,治疗组之间没有差异。
由此可见,艾司西酞普兰治疗焦虑对减少冠心病患者的焦虑是安全和有效的。
参考文献:
Effect of Exercise, Escitalopram, or Placebo on Anxiety in Patients With Coronary Heart Disease: The Understanding the Benefits of Exercise and Escitalopram in Anxious Patients With Coronary Heart Disease (UNWIND) Randomized Clinical Trial. JAMA Psychiatry. Published online August 18, 2021. doi:10.1001/jamapsychiatry.2021.2236
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#Psychiatry#
42
#冠心病患者#
43
学习了,很赞
67
为了积分
60
这个图形摘要和我们以前发的一篇好像啊,哈哈哈
71
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54