第五届呼吸危重症论坛 |《成人经鼻高流量湿化氧疗临床规范应用专家共识》发布:多专家分步解读
2019-03-24 seven MedSci原创
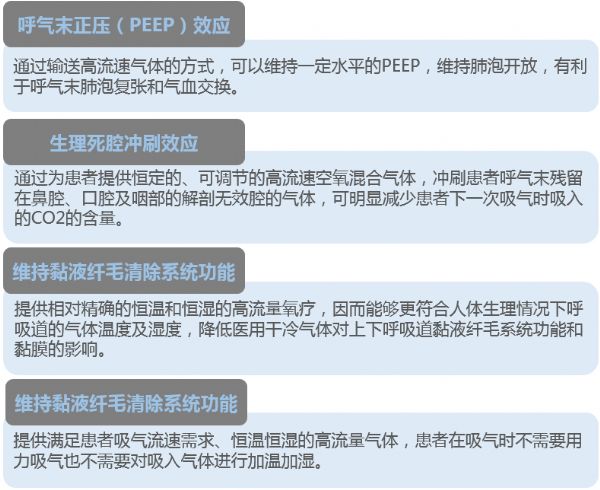
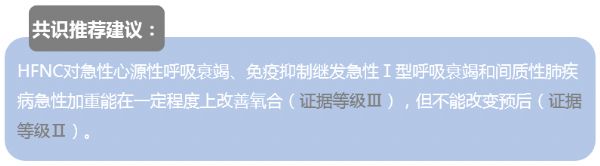
3月23日下午第五届全国呼吸危重症论坛上,我国《成人经鼻高流量湿化氧疗临床规范应用专家共识》发布,且参与共识撰写的多位临床专家对共识进行了解读。推荐亮点:经鼻高流量湿化氧疗(HFNC)能够通过吸入高流量气体产生一定水平的呼气末正压、冲刷上呼吸道生理死腔、恒温恒湿的气体维持黏液纤毛清除系统功能,以及降低患者上气道阻力和呼吸功等作用改善患者的换气和部分通气功能,对单纯低氧性呼吸衰竭(I型呼吸衰竭)
推荐亮点:经鼻高流量湿化氧疗(HFNC)能够通过吸入高流量气体产生一定水平的呼气末正压、冲刷上呼吸道生理死腔、恒温恒湿的气体维持黏液纤毛清除系统功能,以及降低患者上气道阻力和呼吸功等作用改善患者的换气和部分通气功能,对单纯低氧性呼吸衰竭(I型呼吸衰竭)患者具有积极的治疗作用,对部分轻度低氧合并高碳酸血症(II型呼吸衰竭)患者可能也具有一定的治疗作用,但尚需要大样本的临床研究证实。需要指出的是,HFNC的局限性也应正确认识。明确其适应证和禁忌证、规范临床应用势在必行。
HFNC结构及生理学作用机制
解放军总医院第一医学中心 胡兴硕
HFNC按其结构特点可分为3大组成部分:
(1)气体的空氧混合部分:其作用是将空气和氧气按预设氧浓度在涡轮前进行混合。
(2)气体的加温湿化部分:其作用是将空氧混合后的气体进行加温湿化。
(3)气体的输送部分:其作用是保证已完成加温湿化的空氧混合气体以恒温恒湿恒流速的方式输送至患者端。
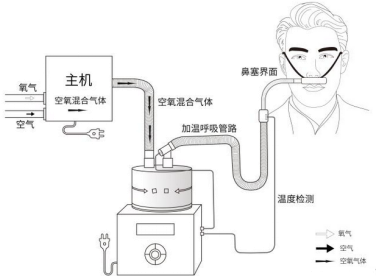
经鼻高流量湿化氧疗仪示意图
高流量湿化氧疗仪与患者连接部分为高流量鼻塞,高流量鼻塞的尖端呈斜面型的出口,质地柔软,用一个具有弹性可调节的过耳头带固定于患者面部。
而HFNC的生理学机制包括以下四个方面:
HFNC应用适应证/禁忌证及临床操作细节问题
中日友好医院 夏金根
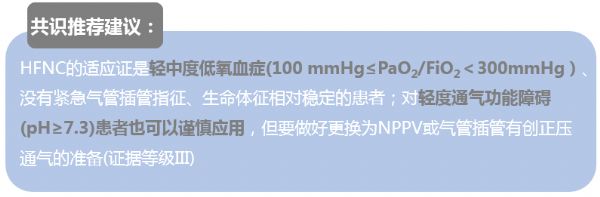
HFNC具体的适应证和禁忌证

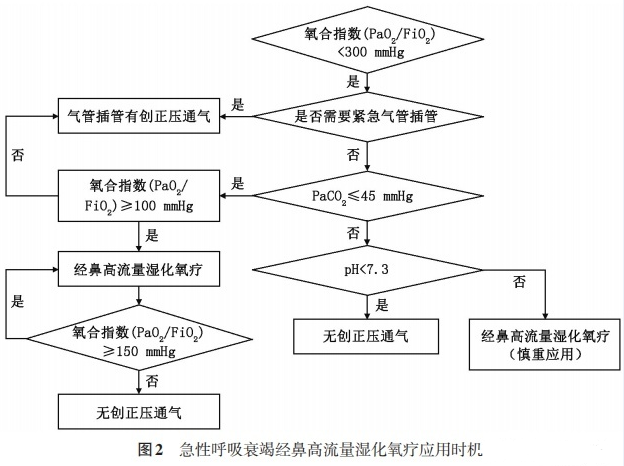
便于临床应用,共识推荐了HFNC的应用时机流程图:
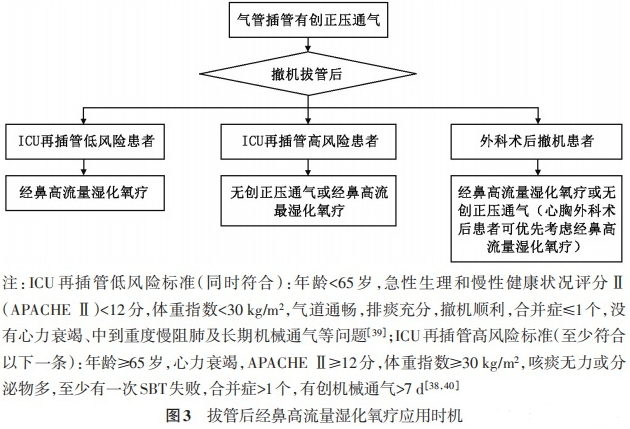
HFNC辅助拔管的治疗时机流程图:
此外,临床中常见的操作问题,关于HFNC的参数设置夏教授建议如下:
I型呼吸衰竭
1. Flow:初始设置30-40 L/min;耐受性
2. FiO2 维持 SpO2 92%-96%
3. 温度(31℃-37℃):依据舒适性及耐受度、痰液粘稠度等
II型呼吸衰竭
1. Flow:初始设置20-30 L/min ,如患者二氧化碳潴留明显,流量设置可考虑在45-55L/min至更高;耐受性
2. FiO2 : 维持 SPO2 88%-92%
3. 温度(31℃-37℃):依据舒适性及耐受度、痰液粘稠度等
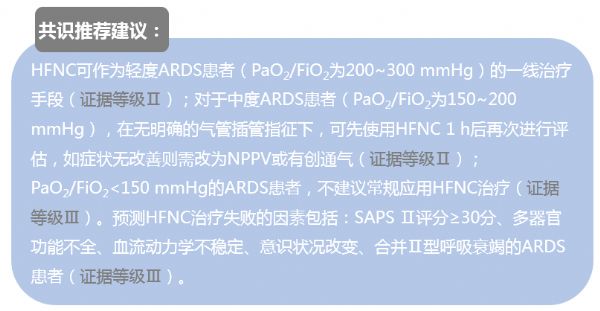
HFNC治疗ARDS:应用与展望
中南大学湘雅医院 潘频华
新共识对HFNC治疗ARDS做了推荐,但很多证据等级还不够高,需要进一步的研究去证实。潘教授对于HFNC治疗ADRS也提出了一些临床问题,希望引起大家的思考:
HFNC治疗ARDS湿度多少合适?
HFNC气管内氧浓度最高可以达到多少?
HFNC联合面罩可以更好的改善氧合?
HFNC流量与产生的PEEP有关,治疗ARDS的流量要不要最高60L/min?
哪种ARDS亚型更适合HFNC治疗?
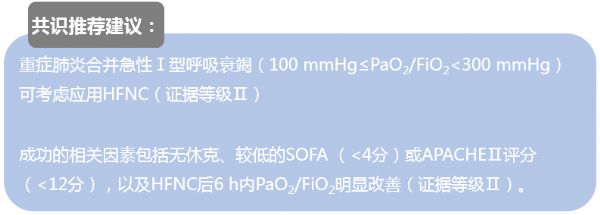
HFNC治疗重症肺炎及其他低氧性呼吸衰竭:时机与问题
空军军医大学 宋立强
宋教授强调针对常规氧疗失败的SCAP,建议大家探索新的成功预测指标——ROX index:指脉氧饱和度与吸氧浓度比值除以呼吸频率(PaO2/FiO2)/RR。
临床上,对于重症肺炎存在基础气道肺病者成功率高,不同病原体肺炎需要个体化的氧疗策略。
临床上,其他急性呼吸衰竭:神经肌肉疾病、急性肺栓塞、支气管镜检查的氧疗、拒绝机械通气者,可以试用HFNC。
血液疾病合并急性呼吸衰竭失败率高,其中肺炎是危险因素。
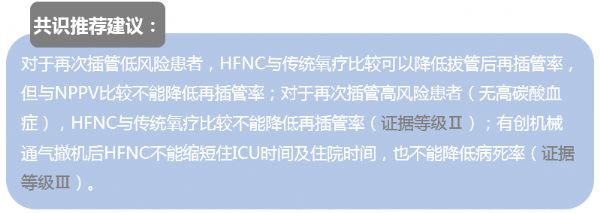
HFNC在有创通气撤机中的地位
海军军医大学附属长海医院 董宇超
董教授强调,机械通气脱机后给予经鼻高流量湿化氧疗序贯能否减少再插管率尚需要进一步研究证实,但可以明显改善患者耐受性,降低痰液粘稠。
经鼻高流量湿化氧疗的核心价值还是温化湿化,轻症患者能给予一定支持,重症患者的支持强度不够。
对于气管切开患者,经气管切开套管给予高流量湿化氧疗,有固有的优势,等待研究证实。
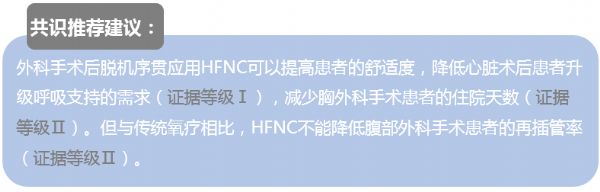
HFNC在外科术后的应用价值
上海交通大学附属瑞金医院 刘嘉琳
刘主任强调,术后呼吸系统并发症(PPC)常见,且相关死亡率及发病率都不低,常见于心脏术后(40%)、胸外术后(30%)、腹部术后(23%)、血管外科术后(6%)。
而无创正压通气临床应用有许多受限因素,如颜面部受损、近期上消化道手术/出血等,这时HFNC治疗在临床应用中,有其明显的优势。现场刘主任列举了多篇高质量研究文献,对HFNC治疗PPC疗效进行论证,所以共识中HFNC在外科术后的治疗中推荐等级高。
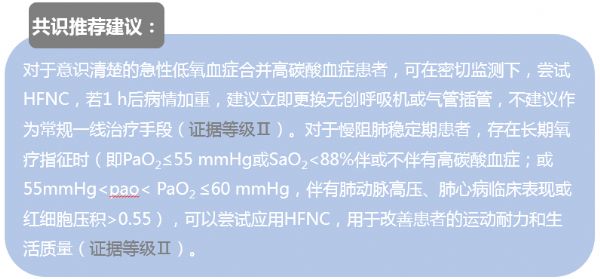
HFNC治疗低氧合并高碳酸血症:临床界限何在
北京大学第三医院 周庆涛
周教授指出,HFNC治疗慢性低氧合并高碳酸血症时,在慢阻肺稳定期,HFNC短期治疗高碳酸血症是安全的,长期治疗能够减少慢阻肺急性加重次数和天数,减少住院次数,改善生活质量,但对肺功能、6min步行距离、呼吸困难症状和氧合的改善目前存在一定分歧。
HFNC与LTOT相比,能够降低PaCO2; HFNC与NPPV相比,改善PCO2疗效相当。
而对于急性低氧合并高碳酸血症患者,主要是慢阻肺急性加重,也包括肺炎、ILD、心衰等,大部分患者为轻中度低氧合并高碳酸血症,HFNC能够改善患者的PCO2,与NPPV相比疗效相当,但耐受性更好。
HFNC作为新的呼吸支持技术在临床得到广泛应用,对轻中度低氧性呼吸衰竭患者具有积极的治疗效果,所以此次共识的发布旨在规范合理使用,对于HFNC明确的适应范围,还需进一步的临床研究。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
40
学习了
56
#规范应用#
45
#专家共识#
35
#成人经鼻高流量湿化氧疗临床规范应用专家共识#
31
#成人经鼻高流量湿化氧疗#
37
#氧疗#
28