JAHA:血栓性闭塞症患者并发症的长期预后和预后因素
2018-12-02 xing.T MedSci原创
由此可见,这项全国范围的研究表明,34%的闭塞性血栓炎患者将在诊断后15年内接受截肢,该研究确定了血管并发症和截肢的高风险患者。
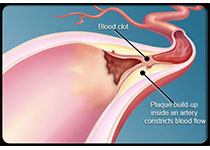
有关血栓闭塞性脉管炎患者长期预后的数据十分缺乏,大多数系列报导来自于印度和日本。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在这项研究中,研究人员评估了一个大型血栓闭塞性脉管炎患者的长期预后和预后因素。
研究人员对符合Papa标准的224例血栓闭塞性脉管炎患者的特征和结局进行了回顾性多中心研究,确定了与血管事件和截肢相关的因素。诊断的中位年龄为38.5(32-46)岁,51名(23.8%)患者为女性,81.7%为白人。
平均随访5.7年后,血管事件发生率为58.9%,截肢率为21.4%,死亡率为1.4%。5年、10年和15年无血管事件的存活率和无截肢存活率分别为41%和85%、23%和74%以及19%和66%。种族(非白人)(风险比为2.35[1.30-4.27],P=0.005)和诊断时的肢体感染(风险比为3.29[1.02-10.6],P=0.045)是血管无事件生存的独立因素。与截肢相关的因素为肢体感染(风险比为12.1[3.5-42.1],P<0.001)。停止吸烟的患者截肢风险较低(P=0.001)。
由此可见,这项全国范围的研究表明,34%的闭塞性血栓炎患者将在诊断后15年内接受截肢,该研究确定了血管并发症和截肢的高风险患者。
原始出处:
Alexandre Le.et al.Long‐Term Outcome and Prognostic Factors of Complications in Thromboangiitis Obliterans (Buerger's Disease): A Multicenter Study of 224 Patients.JAHA.2018.https://doi.org/10.1161/JAHA.118.010677
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#并发#
30
#血栓性#
23
#血栓性闭塞症#
21
#长期预后#
19
#AHA#
20
#预后因素#
25
学习
51