JCO:当红明星“液态活检”遭遇尴尬!?
2018-03-13 Mackaay 肿瘤资讯
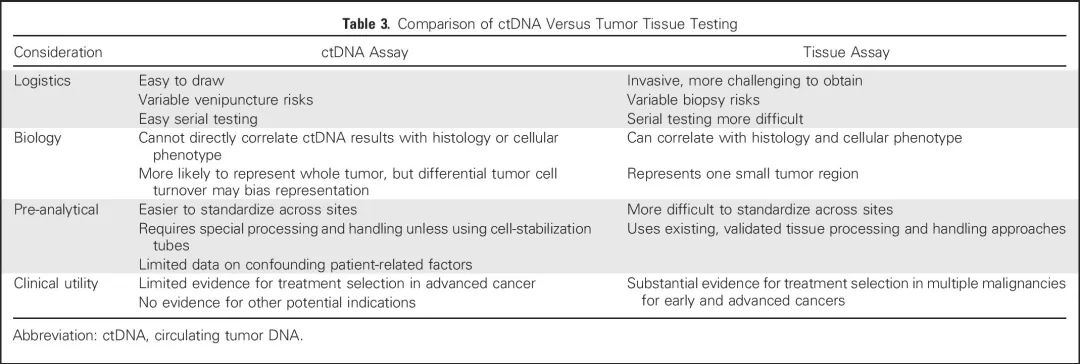
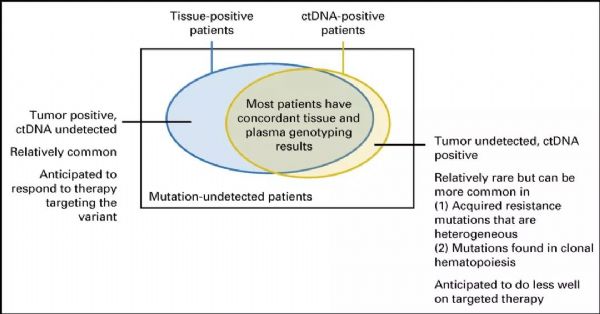
“液态活检”,其主要作用是通过检测血液等体液样本中的ctDNA(循环肿瘤DNA),达到对疾病诊断和监控的作用,最近几年可谓红的发紫,是大量商业广告和公众关注的对象。为此,美国临床肿瘤学会(ASCO)和美国病理学家协会(CAP)专家认为有必要擦亮双眼,采用循证方法对ctDNA检测的结果进行客观汇总分析,理性看待液态活检。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCO#
0
#尴尬#
53
#液态活检#
39
讲的好.液态活检也许是种好手段
92
说的好.也许在临床上有大作用
89
学习学习学习
78
学习学习学习
80
#活检#
41
学习学习学习
68