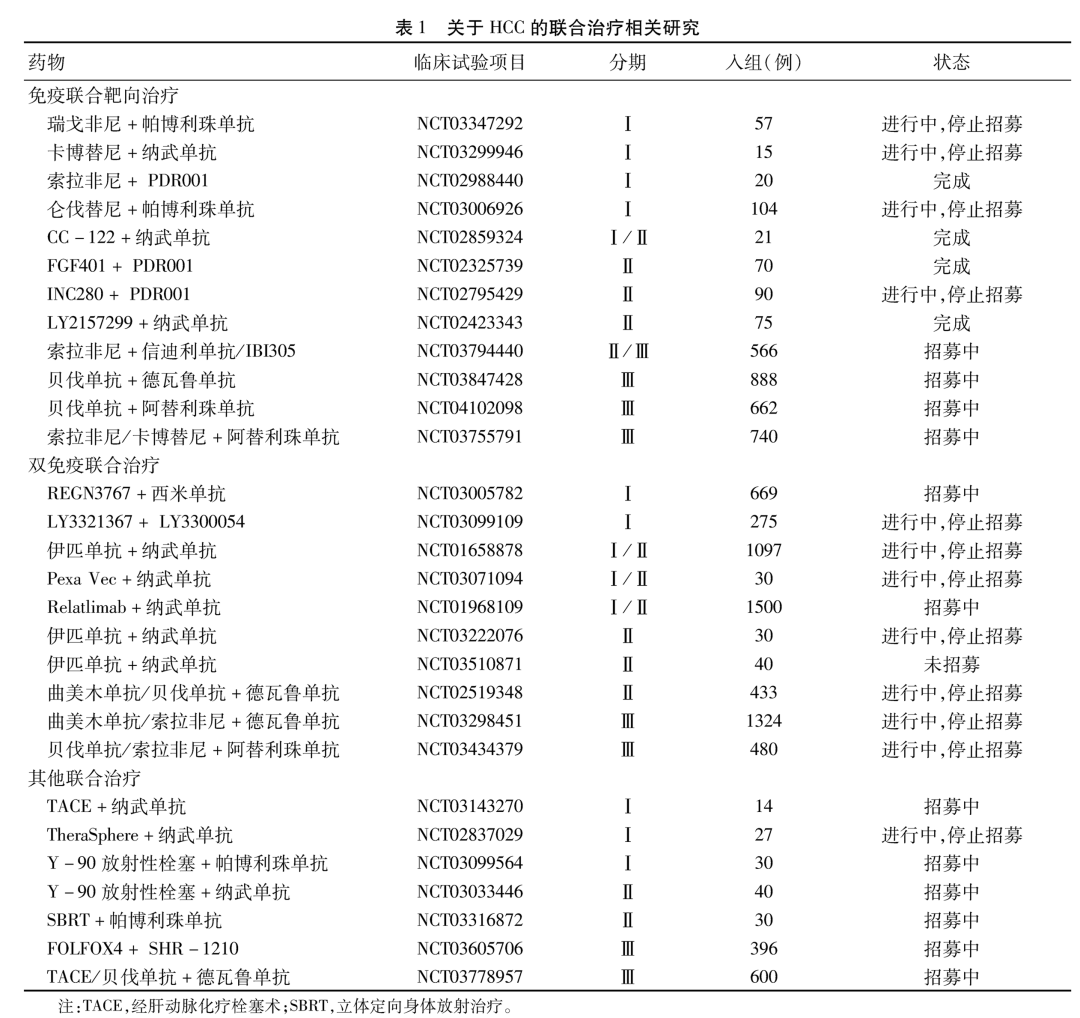
Liver Cancer:肝细胞癌伴有血管侵犯的患者手术切除和系统性治疗的疗效比较
2021-05-19 yd2015 MedSci原创
HCC患者伴有血管侵犯,接受手术切除较系统治疗能够延长患者的OS。
肝细胞癌(HCC)是恶性肿瘤导致死亡的第四大原因。HCC的治疗不仅关注肿瘤的大小、血管侵犯和肝外转移,还有关注患者的体能状态和肝功能分级。目前巴塞罗那分期(BCLC)以及香港肝癌分期在国际上常用于指导肝癌各个分期的治疗。手术切除是HCC患者的治愈性手段,获得5年生存期超过60%。但是临床上只有很少一部分人适合手术。在美国的很多肿瘤机构中,HCC患者伴有血管侵犯,不管程度,都是手术切除的禁忌征;然而来自亚洲的数据表明,伴有乙肝病毒感染的HCC患者,即使伴有血管侵犯,仍有部分患者能够从手术中获益。但是我们知道,西方肝癌的发病原因以及并发症跟亚洲人群有所差别,目前对于这类患者的手术治疗数据有限。因此,来自美国的团队在Liver Cancer杂志上发表了一项研究结果,评估HCC患者伴有血管侵犯手术切除和系统治疗的疗效,以及跟手术切除相关的因素。
研究纳入患者来自国家肿瘤数据库(NCDB),2010年至2017年AJCC 第7版分期为T3BNOM0的HCC患者。共11,259例诊断为T3BN0M0 HCC患者, 分别有325例患者(2.9%) 和 4,268例患者 (37.9%)接受手术切除和系统性治疗。肝叶切除术(43.1%)是最常见的手术切除类型,其次是楔形或节段性切除术(33.5%)和扩大肝叶切除术(17.5%)。85.4%患者伴有AFP的升高。手术切除的患者伴有肝硬化的较系统治疗患者的少。
多因素分析表明,女性患者的生存期(OS)较男性明显延长(调整的HR(AHR)=0.873, 95% CI: 0.793–0.962);另外, AFP升高(AHR: 1.278, 95% CI: 1.132–1.443) 、更高的MELD评分 (AHR per 10 units: 1.137, 95% CI: 1.084–1.193)和肿瘤大小(AHR: 1.011, 95% CI: 1.007–1.015)是HCC伴有血管侵犯患者的危险因素。

HCC伴有血管侵犯手术或系统治疗的危险因素
手术切除对OS的影响:30天内再次入院比例和死亡率分别为10.2和8.5%。一线治疗中手术切除对比系统治疗的中位OS为21.4个月和8.1个月(AHR=0.496, 95% CI: 0.426–0.578)。而且,亚组分析表明,非肝硬化患者(AHR=0.550, 95% CI: 0.326–0.926)以及肝硬化患者(AHR: 0.460, 95% CI: 0.311–0.679)中手术切除均较系统治疗明显延长患者的OS。
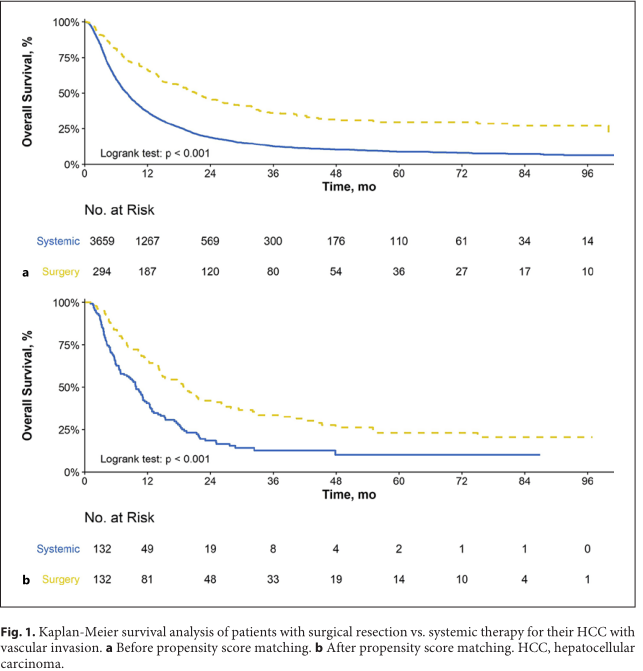
手术切除和系统治疗对生存影响
手术切缘对OS的影响:R0(完全切除)切除患者的中位OS为22.2个月,R1(显微镜下残留)切除患者的中位OS为16.0个月,R2(肉眼残留)切除患者的中位OS为13.2个月,三组有明显统计学差异(P=0.019)。R1切除的患者仍然较系统治疗患者延长生存 (AHR: 0.558, 95% CI 0.381–0.819)。

手术切缘对生存的影响
另外,亚洲人群更多人接受手术切除,而Charlson合并症≥3、甲胎蛋白升高、肿瘤体积较小、社区癌症项目护理、南部或西部地区接受手术切除的比例较低。
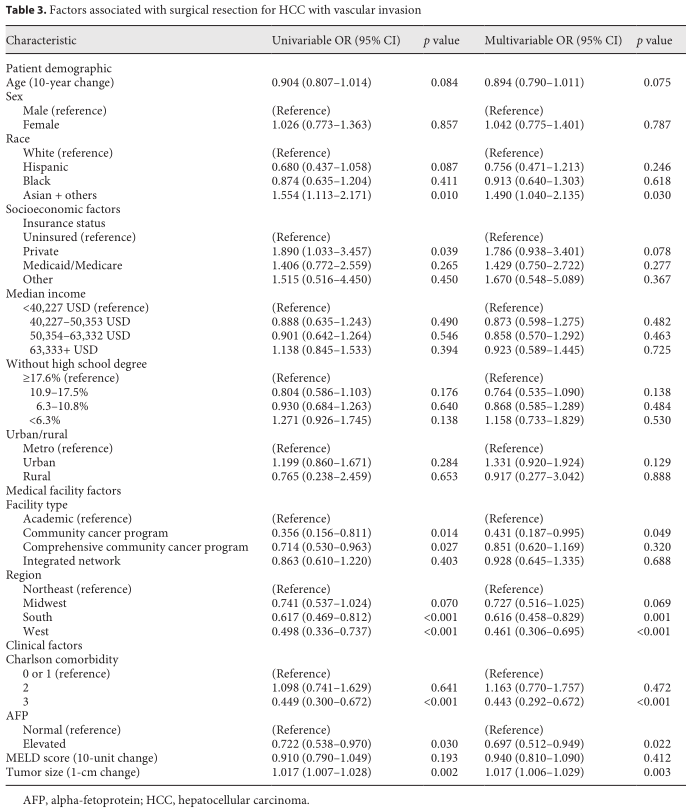
影响选择治疗方式的因素
综上,HCC患者伴有血管侵犯,接受手术切除较系统治疗能够延长患者的OS。
原始出处:
Rajalakshmi Govalan, Marie Lauzon, Michael Luu, et al. Comparison of Surgical Resection and Systemic Treatment for Hepatocellular Carcinoma with Vascular Invasion: National Cancer Database Analysis. Liver Cancer. 2021. DOI: 10.1159/000515554.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞癌#
36
#系统性#
46
#系统性治疗#
43
#肝细胞#
43
#手术切除#
53
谢谢梅斯提供这么好的信息,学到很多
53
好
51