JCO:帕博利珠单抗一线治疗进展期肾透明细胞癌患者一线治疗的ORR可达36.4%
2021-02-03 MedSci原创 MedSci原创
帕博利珠单抗一线治疗进展期肾透明细胞癌(ccRCC)患者安全有效,且反应持久(ORR,36.4%; CR,3.6%; PR,32.7%)。
帕博利珠单抗一线治疗进展期肾透明细胞癌(ccRCC)患者安全有效,且反应持久(ORR,36.4%; CR,3.6%; PR,32.7%)。2月2日,Journal of Clinical Oncology在线发布一项帕博利珠单抗单药治疗ccRCC患者的开放标签、单臂、临床Ⅱ期研究结果。该研究旨在研究PD-1抑制剂帕博利珠单抗单药治疗在未接受过全身抗癌治疗的复发性或晚期或转移性ccRCC患者中的疗效和安全性。
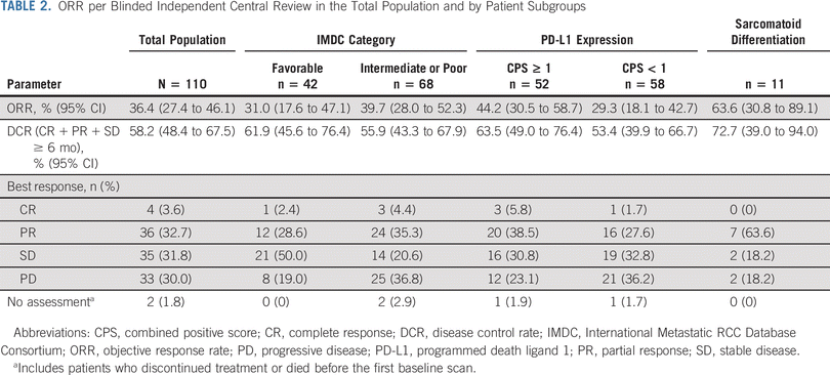
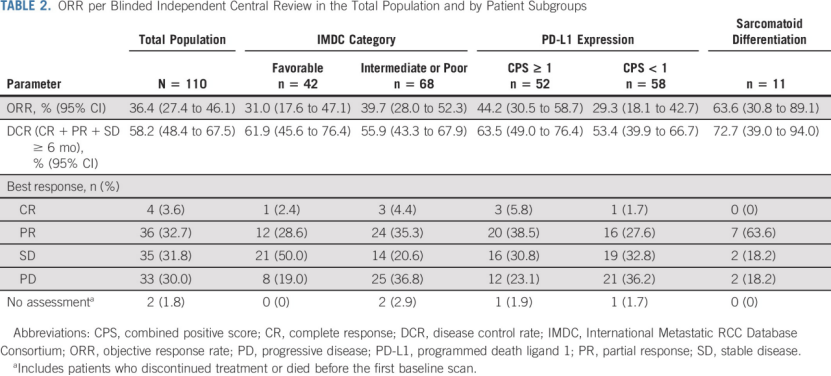
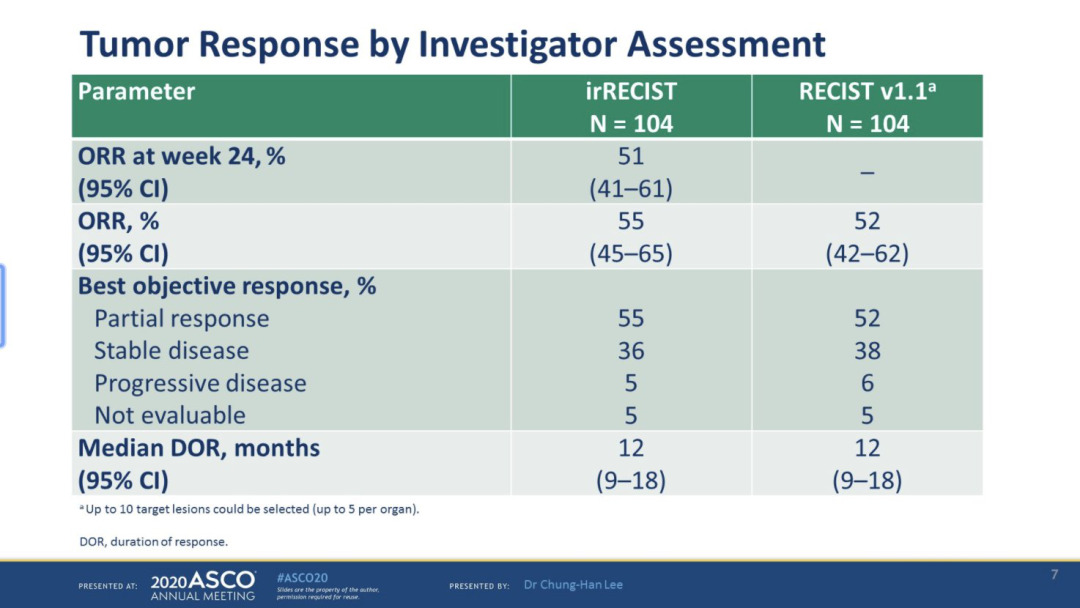
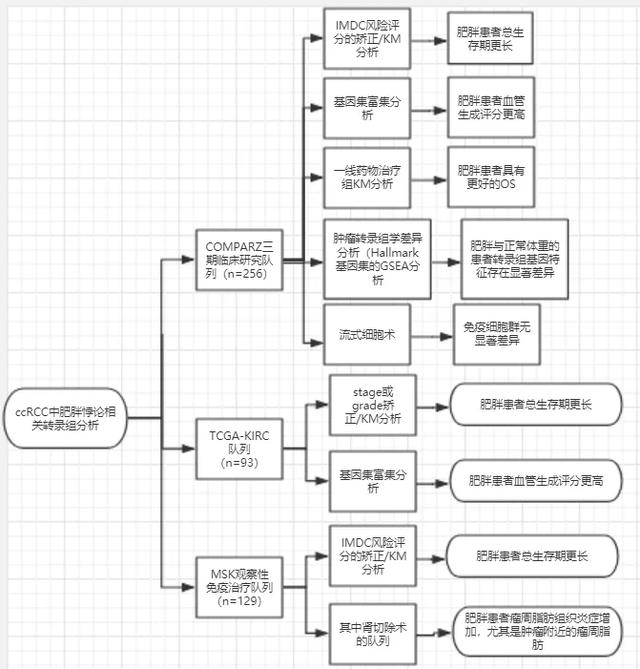
研究共纳入110名患者,ORR为36.4%(95%CI,27.4至46.1),其中4名(3.6%)完全缓解,36名(32.7%)部分缓解。疾病控制率为58.2%(95% CI=48.4-67.5)。大多数患者(68.2%,75/110)病灶减少,其中有30.9%(34/110)患者病灶减少60%。
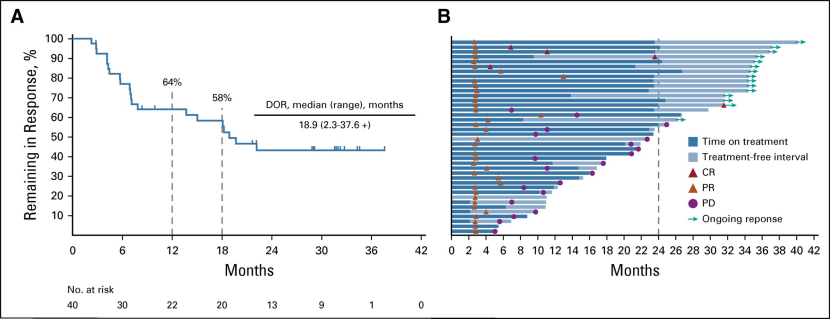
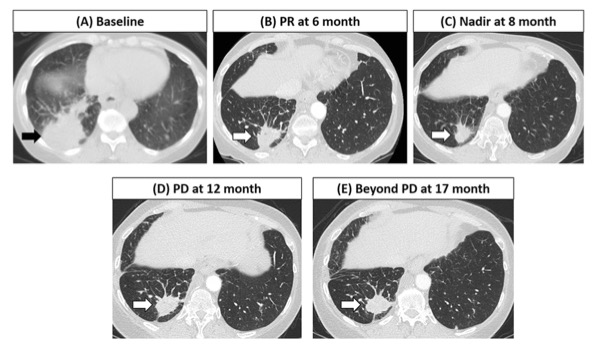
中位缓解持续时间为18.9个月;64.1%响应者的缓解时间超过12个月。中位无进展生存期为7.1个月(95% CI=5.6-11.0),12月PFS率为37.6%,而24月PFS率为22.3%。未达到中位OS,12月和24月OS率分别为88.2%和70.8%。

有42名患者具有良好IMDC风险,68名患者有中等或不良IMDC风险。IMDC风险类别的疗效结果显示,良好IMDC风险组的ORR为31.0%(95%CI,17.6至47.1),其中有1例(2.4%)完全缓解,12例(28.6%)部分缓解。中等或不良IMDC风险组的ORR为39.7%(95%CI,28.0至52.3),其中有3例(4.4%)完全缓解和24例(35.3%)部分缓解。
有52名患者的CPS≥1,58名患者的CPS<1。PD-L1表达的疗效结果显示,CPS≥1组的ORR为44.2%,CPS<1组的ORR为29.3%
30.0%的患者出现3-5级治疗相关不良事件,其中最常见的是结肠炎(5.5%)和腹泻(3.6%)。3例患者因不良事件死亡,还有1例患者死于与治疗有关的肺炎。
尽管单臂设计存在固有的局限性,但这项研究结果表明,对于晚期ccRCC患者(包括所有IMDC风险组)和所有患有IMDC风险的患者,帕博利珠单抗单一疗法具有令人信服的抗肿瘤活性,安全又持久。帕博利珠单抗单药治疗有潜力成为对其他药物耐受较差的晚期ccRCC患者的治疗方法。
这些结果为在晚期或转移性ccRCC患者中进一步探索帕博利珠单抗单药治疗、辅助治疗和基于此的联合治疗提供了支持。
参考资料:David F. McDermott, Jae-Lyun Lee, Georg A. Bjarnason, et al. Open-Label, Single-Arm Phase II Study of Pembrolizumab Monotherapy as First-Line Therapy in Patients With Advanced Clear Cell Renal Cell Carcinoma. February 02, 2021. DOI: 10.1200/JCO.20.02363 Journal of Clinical Oncology.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#透明细胞癌#
48
#细胞癌#
40
#进展期#
47
#JCO#
43
#帕博利珠#
47
#ORR#
39
这些结果为在晚期或转移性ccRCC患者中进一步探索帕博利珠单抗单药治疗、辅助治疗和基于此的联合治疗提供了支持。
91
PPd-PPd-1
89