Transl Lung Cancer Res: 基线肿瘤大小(BTS)与NSCLC接受免疫单药或联合化疗患者预后的关系
2022-03-17 yd2015 网络
研究表明,大max BTS是接受免疫单药治疗患者PFS较差的预后因素,但在接受免疫联合化疗治疗患者中没有预测作用。
基线肿瘤大小(BTS)是接受免疫检查点抑制剂单药治疗(ICI-mono)的非小细胞肺癌(NSCLC)患者的预后因素。然而,在接受ICI联合化疗(ICI-chemo)的患者中,这种关系尚不清楚。近期,来自日本的团队开展了相关研究,相关结果发表在Translational Lung Cancer Research杂志上。
这项单中心回顾性研究评估了159名2016年1月至2021年4月接受一线免疫检查点抑制剂单药治疗(ICI-mono)或ICI联合化疗(ICI-chemo)的晚期NSCLC患者。根据实体肿瘤应答评价标准进行影像学评估,使用最大靶病灶最长直径(maxi BTS)和总靶病灶最长直径(total BTS)估算其BTS值。
研究最终纳入159例患者,共有80例(50.3%)患者接受了ICI-mono, 79例(49.7%)患者接受了ICI-chemo。中位年龄71岁(31-89岁),80.5%的患者为男性。104例(65.4%)为腺癌,38例(23.9%)为鳞状细胞癌,17例(10.7%)为非特异性(NOS)癌。143例(89.9%)患者可知PD-L1水平,其中86例(54.1%)患者发现PD-L1肿瘤比例评分(TPS)≧50%。所有患者中位max BTS、总BTS、受检器官数分别为54.2(37.2-72.5)mm、104.3(67.7-151.1)mm、3.0 (IQR, 2.0-4.0)。
ICI-mono组患者中,中位无进展生存期(PFS)在小max BTS组为16.7个月(95% CI: 10.7-NA),在大max BTS组为3.3个月(95% CI: 1.4-9.9)(HR, 0.39;95%CI:0.22 0.70;P = 0.0012a)。小的总BTS组的中位PFS为11.8个月(95% CI: 9.9-25.5),大的总BTS组的中位PFS为2.4个月(95% CI: 1.2-8.3)(HR: 0.38;95%CI:0.22 0.65;p<0.001)。中位PFS在少数器官受累组为10.7 (95% CI: 5.8-16.7)个月,在大量器官受累组为2.1 (95% CI: 1.2-NA)个月(HR, 0.43;95%CI:0.21-0.88;P = 0.0053)。在PD-L1 TPS≥50%的患者中,小max BTS组的中位PFS为22.5 (95% CI: 11.0-NA)个月,大max BTS组的中位PFS为4.5 (95% CI: 2.1-10.8)个月(HR, 0.40;95%CI:0.20-0.77;P = 0.0049)。小max BTS组的中位OS未达到,但大max BTS组的中位OS达到12.1个月(95% CI: 9.0-25.5)(HR, 0.39;95%CI:0.19 0.78;P = 0.0065)。
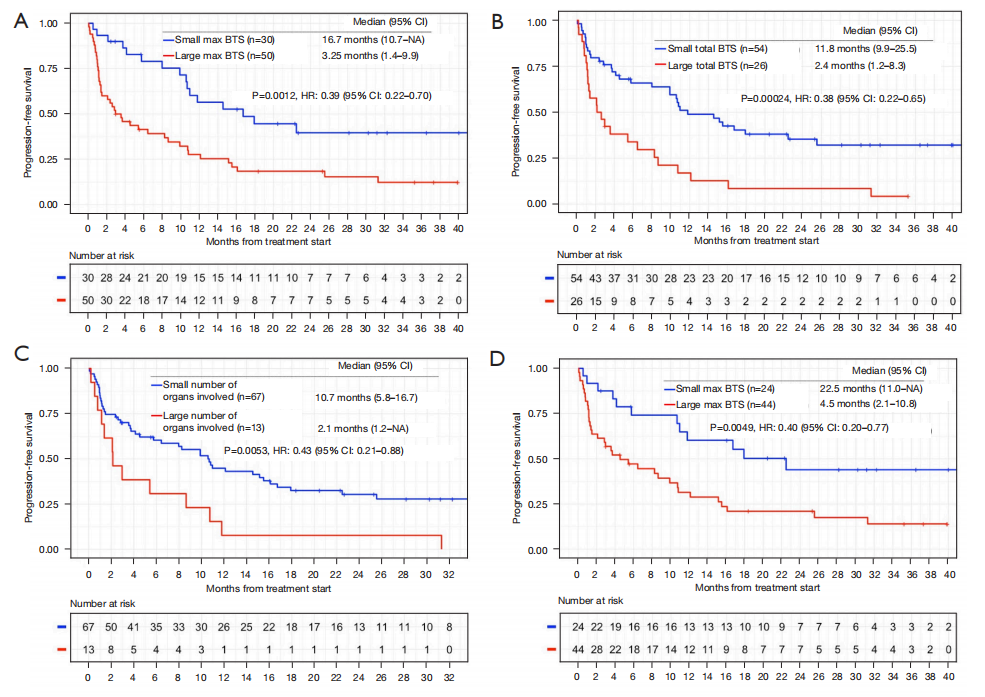
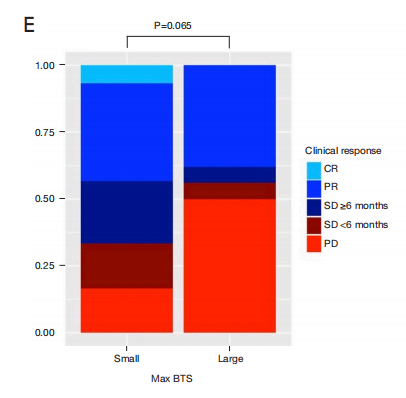
小max BTS组的CBR高于大max BTS组(67.7% vs. 44.0%;P = 0.065)。小max BTS组的疾病控制率(DCR)显著高于大max BTS组(83.4% vs 50.0%;P = 0.004)。
ICI-chemo组患者中,中位无进展生存期(PFS)在小max BTS组为7.8个月(95% CI: 6.4-14.3),在大max BTS组为15.6个月(95% CI: 6.3-NA),差异无统计学意义(P=0.21)。小总BTS组中位PFS为10.4个月(95% CI: 7.0 17.1), 大总BTS组中位PFS为4.4个月(95% CI: 3.0-NA),差异无统计学意义(P=0.062)。中位PFS在少数器官受累组为11.5个月(95% CI: 7.8 19.9),在大量器官受累组为5.2个月(95% CI: 3.7 14.2),差异无统计学意义(P=0.064)。PD-L1 TPS≧50%的患者,小max BTS组的中位PFS为17.1个月(95% CI: 10.1-NA),大max BTS组的中位PFS为15.7个月(95% CI: 7.7-NA),差异无统计学意义(P=0.74)。

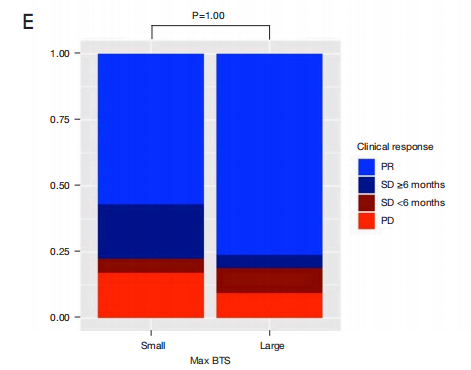
小、大max BTS组间CBR无显著差异(77.6% vs. 80.1%;P = 1.00)。小、大max BTS组间DCR也无显著差异(DCR, 82.8% vs. 90.5%;P = 0.494)。
max BTS ≥50 mm患者中,中位PFS在ICI-mono组为3.6个月(95% CI: 1.4-9.9),而在ICI-chemo组为10.6个月(95% CI: 6.5 -15.7)(HR: 0.59;95%CI:0.36 0.96;P = 0.032)。CI-mono组的中位OS为15.2个月(95% CI: 9.3-25.5),而CI-chemo组的中位OS未达到(HR, 0.56;95%CI:0.31 1.04;P = 0.065)。在PD-L1 TPS≧50%的患者中,ICI-mono组的中位PFS为4.5个月(95% CI: 2.1-10.8),而ICI-chemo组的中位PFS为15.7个月(95% CI: 7.7 NA)(HR, 0.38;95%CI:0.14 1.10;P = 0.064)。在PD-L1 TPS≧50%的患者中,CI-mono组的中位OS为15.6个月(95% CI: 9.3 -34.7),而CI-chemo组尚未达到,差异无统计学差异(P=0.32)。

综上,研究表明,大max BTS是接受免疫单药治疗患者PFS较差的预后因素,但在接受免疫联合化疗治疗患者中没有预测作用。
原始出处:
Uehara Y, Hakozaki T, Kitadai R, Narita K, Watanabe K, Hashimoto K, Kawai S, Yomota M, Hosomi Y. Association between the baseline tumor size and outcomes of patients with non-small cell lung cancer treated with first-line immune checkpoint inhibitor monotherapy or in combination with chemotherapy. Transl Lung Cancer Res. 2022 Feb;11(2):135-149. doi: 10.21037/tlcr-21-815. PMID: 35280320; PMCID: PMC8902087.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TRA#
51
#Transl#
51
#患者预后#
53
感谢分享
33
#联合化疗#
53