JACC:老年患者皮下或经静脉植入式心律转复除颤器的长期结果
2022-03-21 网络 网络
心律失常导致的心脏性猝死(SCD)是心血管死亡的主要原因,占全球50%以上的心血管死亡事件。
心律失常导致的心脏性猝死(SCD)是心血管死亡的主要原因,占全球50%以上的心血管死亡事件。许多大型临床试验发现,埋藏式心脏转复除颤器(ICD)可降低特定人群的SCD死亡率。
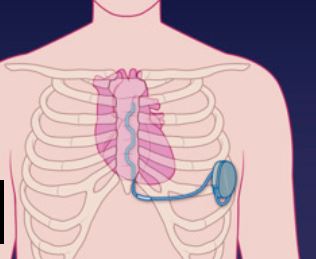
通常,心脏除颤或心脏复律波形能量控制系统采用经静脉ICD或皮下S-ICD治疗心脏心律失常。但传统的经静脉ICD有经静脉导线的固有缺点,包括:置入导线时的风险–心脏穿孔、心包积液、心包填塞、血胸、气胸;以及装置寿命期限内的延迟风险–血管内导线感染、导线故障等。
植入式心律转复除颤器或自动植入式心律转复除颤器是可植入体内的设备,能够执行除颤,并且取决于心脏的类型,心脏复律和起搏。对于因室颤和室性心动过速而有心源性猝死风险的患者,ICD是一线治疗和预防性治疗。

皮下(S-)植入式心律转复除颤器(ICD)是经静脉(TV-)ICD的替代品,越来越多地被植入年轻患者体内;目前还缺乏S-ICD在老年患者中的安全性和有效性数据。为此,来自杜克大学医院电生理科的专家比较接受S-ICD或TV-ICD的老年患者的结果并发表在JACC杂志上。
结果共研究了16063名患者(年龄72.6±5.9岁,28.4%为女性,射血分数28.3±8.9%)。与TV-ICD患者(n = 15072)相比,S-ICD患者(n = 991,总体6.2%)更经常是黑人,更年轻,更依赖透析,更不可能有心房颤动或扑动史。
在调整后的分析中,设备类型与全因死亡率(HR:1.020;95%CI:0.819-1.270)、设备再手术(HR:0.976;95%CI:0.645-1.479)、因感染而拆除设备(sHR:0. 614;95% CI:0.138-2.736),无感染的设备再手术(sHR:0.975;95% CI:0.632-1.506),心血管疾病再入院(sHR:1.087;95% CI:0.912-1.295),或复发性全因再入院(HR:1.072;95% CI:0.990-1.161)均无关。

综上,S-ICD和TV-ICD接受者的死亡、装置再手术、因感染而移除装置、无感染的装置再手术以及心血管疾病和全因再入院的风险相似。
参考文献:
Longitudinal Outcomes of Subcutaneous or Transvenous Implantable Cardioverter-Defibrillators in Older Patients. J Am Coll Cardiol. 2022 Mar, 79 (11) 1050–1059
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#JACC#
59
#长期结果#
43
#心律转复除颤器#
33
#植入式#
46
#静脉#
32
#ACC#
31
#植入式心律转复除颤器#
41
#除颤#
34
#植入#
59