Neurology:SIH患者持续性脊髓腹侧CSF漏的长期风险:浅表铁质沉着症和双臂肌萎缩
2021-09-23 Naomii MedSci原创
在51例持续脊髓脊液腹侧漏的低颅压患者的持续随访中发现,发展成严重的长期后遗症的风险是相当大的。早期腹侧脑脊液漏的治疗提供了一个绝佳的治疗时机,可预防浅表含铁血黄素沉着症、双臂肌萎缩所致的神经功能障碍
自发性低颅压(SIH)已成为公认的继发性头痛的原因。脊椎水平的自发性脑脊液(CSF)渗漏是SIH的原因。随着影像学的进展,目前至少发现了至少3种自发性脑脊液渗漏——位于脊髓腹侧或背侧的硬脑膜撕裂的Ⅰ型渗漏、单纯型或复合型脑膜憩室相关的Ⅱ型渗漏、静脉瘘的Ⅲ型渗漏。约四分之一的SIH患者有腹侧脑脊液漏,由于位置在脊髓腹侧且几乎无处不在地存在骨刺,这些渗漏通常对保守治疗,传统的硬膜外治疗是难治的,因此这些渗漏有成为慢性的倾向,患处浅表含铁血黄素沉着症、双臂肌力减退和脊髓突出症是少见但严重的长期后遗症。目前尚无针对这一慢性病变的研究,研究人员对持续性脊液腹侧漏患者的后遗症风险进行了量化。
这是一项前瞻性的队列研究,患者符合修改后的国际头痛疾病分类(ICHD)-III的SIH标准。患者群体由一组连续的SIH和持续性脊髓脊液腹侧漏患者组成。他们在SIH症状出现后一年内诊断并入组,并进行至少一年的随访。
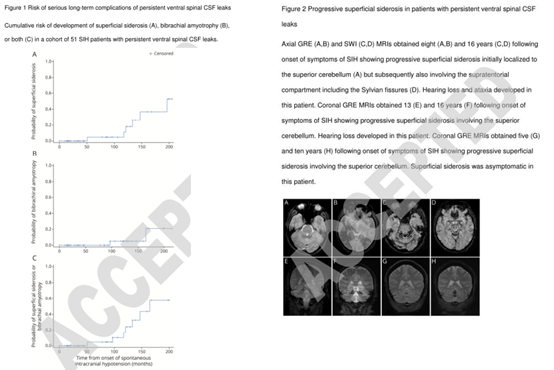
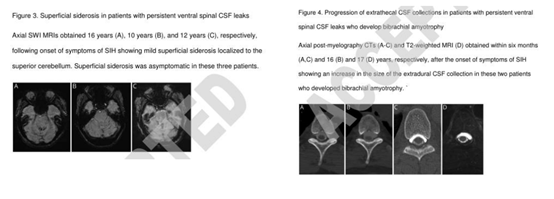
在51例持续脊髓脊液腹侧漏的低颅压中,在280个患者-随访年期间,6例患者出现了浅表铁质沉着症,2例患者出现了双臂肌萎缩症。这些并发症的发生概率从48个月的0%上升到56个月的4.5%(95%可信区间:1.0-28.0%),96个月的10.5%(95%可信区间:3.0-36.4%),144个月的32.7%(95%可信区间:15.0-62.8%),192个月的57.9%(95%可信区间:30.2-87.6%)。所有患者均未发生脊髓突出症。
在SIH并持续存在脊髓腹侧脑脊液漏的患者中,发展成严重的长期后遗症的风险是相当大的。这项研究表明,早期对腹侧脑脊液漏的治疗提供了一个绝佳的治疗时机,可以预防浅表含铁血黄素沉着症和双臂肌萎缩所致的神经功能障碍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CSF#
33
#SIH#
29
#萎缩#
30
#持续性#
40
#Neurol#
31
#长期风险#
37
#肌萎缩#
31