Movement disorders:帕金森患者,葡萄糖和脂质代谢异常,痴呆风险更高
2022-02-19 Freeman MedSci原创
GBA和APOE基因分型可以改善对PD认知能力下降的预测
帕金森病(PD)患者比健康的老年人更容易出现认知能力下降。认知方面的问题影响了患者的工作和独立运作的能力,使他们处于生活质量差和被安置在养老院的更高风险中。PD的认知症状的演变是非常异质的,阻碍了招募相关参与者进入临床试验。因此,识别认知缺陷高风险患者的方法将大大改善未来试验的设计和成本。

遗传因素是预测PD(PDD)认知能力下降和痴呆的候选因素,尽管已发表的研究设计中的异质性导致了不一致的发现。其中最有力的候选因素是脂蛋白E(APOE)、β-葡萄糖苷酶(GBA)、微管相关蛋白tau(MAPT)和α-突触核蛋白(SNCA)位点的变异。APOE的ε4等位基因(APOE-ε4)是散发性阿尔茨海默病(AD)最强的遗传风险因素,也是路易体痴呆(DLB)全基因组关联研究中的佼佼者,一些大型研究显示它对PD认知能力下降的进展有影响。
GBA突变是PD最常见的遗传风险因素,而且GBA突变携带者的痴呆风险受突变类型的影响。H1 MAPT单倍型与包括AD在内的tauopathies有关,也与PD有关,SNCA的常见变异是散发性PD的既定危险因素。一些研究表明,SNCA和MAPT的变异也可能影响PD的认知能力下降,尽管结果并不一致。
尽管关于APOE、GBA、MAPT和SNCA中的遗传变异对PD认知进展的影响的文献很多,但从PD诊断时起进行前瞻性随访的大型研究很少,许多研究仅从临床环境中追踪患者。
藉此, 挪威Stavanger University Hospital的Aleksandra A. Szwedo等人,探究了APOE、GBA、MAPT和SNCA位点在帕金森病发病率队列协作组(PICC)的自然过程中对全球认知能力下降和痴呆症发展的重要性。这六个纵向的、以人口为基础的欧洲队列共同构成了一个大样本,其中包括从诊断为帕金森病时起长达10年的疾病进展的特征。
他们对1002名PD患者进行了长达10年(中位数7.2年)的随访,对APOE-ε4、GBA突变、MAPT H1/H2或SNCA rs356219中的至少一种进行了基因分型。用线性混合模型评估了基因型对认知能力下降率(Mini-Mental State Examanation, MMSE)的影响,用Cox回归评估了痴呆症的发展(用标准化标准诊断);用Benjamini-Hochberg校正法对多重比较进行了说明。
他们发现:APOE-ε4(n = 281, 29.7%)和GBA突变(n = 100, 10.3%)的携带者比非携带者有更快的认知衰退和更高的痴呆进展风险(APOE-ε4,HR 3.57, P < 0.001;GBA突变,HR 1.76, P = 0.001)。
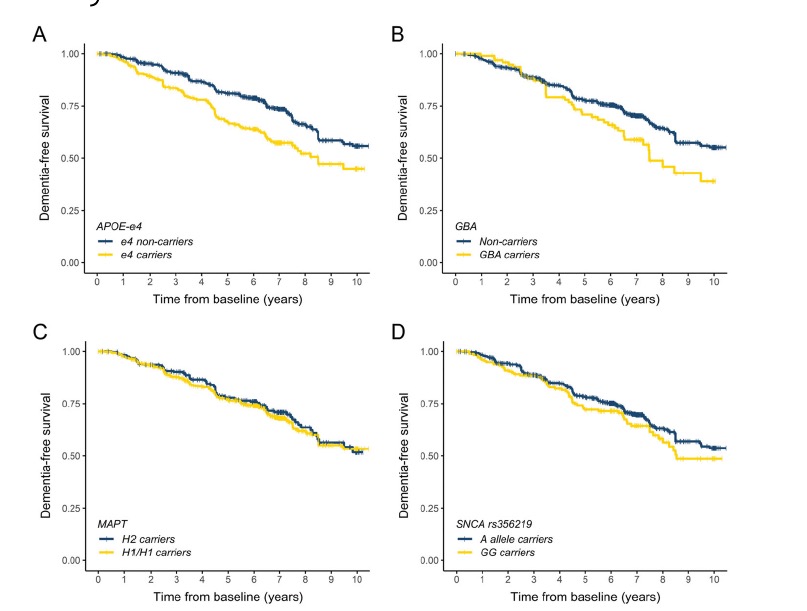 两种风险基因型的携带者(n = 23)的认知能力下降和痴呆的风险(HR 5.19,P < 0.001)进一步增加。没有观察到MAPT或SNCA rs356219的明显影响。
两种风险基因型的携带者(n = 23)的认知能力下降和痴呆的风险(HR 5.19,P < 0.001)进一步增加。没有观察到MAPT或SNCA rs356219的明显影响。
该研究的重要意义在于发现了:GBA和APOE基因分型可以改善对PD认知能力下降的预测,这对于为临床试验的选择提供信息非常重要,并有可能实现个性化治疗。
原文出处:
[Szwedo AA, Dalen I, Pedersen KF, et al. GBA and APOE Impact Cognitive Decline in Parkinson’s Disease: A 10‐Year Population‐Based Study. Movement Disorders. Published online February 2, 2022:mds.28932. doi:10.1002/mds.28932](https://doi.org/10.1002/mds.28932)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Dis#
41
#disorders#
33
#ERS#
34
#disorder#
35
#Disord#
37
#痴呆风险#
31
#脂质代谢#
50
#代谢异常#
34
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
31