新型取栓技术(SPACEMAN)的技术考虑和应用场景:一项前瞻性研究
2022-03-07 吴迎春 网络
对于急性大血管闭塞性病变所致的脑梗死,机械取栓术已经是标准化治疗。对于亚洲及非洲人群而言,颅内动脉粥样硬化(ICAS病变)是导致脑梗死最常见的原因,尤其对于中国人群。
第一作者:吴迎春1
通讯作者:吴迎春
其他作者:王俊梅 孙瑞 冯冠清 李文钊 桂月江 郑艳安
作者单位:鄂尔多斯市中心医院神经内科
基金项目:鄂尔多斯市产业园创新人才团队
[REF: Wu Y, Wang J, Sun R, Feng G, Li W,Gui Y and Zheng Y (2022) A Novel Endovascular Therapy Strategy for Acute Ischemic Stroke Due to Intracranial Atherosclerosis-Related Large Vessel Occlusion: Stent-Pass-Aspiration-resCuE-micowire-Angioplasty (SPACEMAN) Technique. Front. Neurol. 13:798542. doi: 10.3389/fneur.2022.798542
研究背景
对于急性大血管闭塞性病变所致的脑梗死,机械取栓术已经是标准化治疗。对于亚洲及非洲人群而言,颅内动脉粥样硬化(ICAS病变)是导致脑梗死最常见的原因,尤其对于中国人群。然而有接近30%的急性脑梗死患者接受不到再灌注治疗,这也导致了脑梗死患者预后差的原因之一。部分患者取栓术失败率高,这点可能预示颅内动脉硬化为此类患者脑梗死病因。ICAS病变患者需要更多的取栓次数及更长的手术时间。更严重的是,ICAS病变导致的大血管闭塞患者,应用传统技术进行取栓,术中约1/3患者会发生再闭塞。因此对于ICAS病变导致的急性大血管闭塞,新型取栓技术的探索更显得尤为重要。同时对于术中再闭塞的补救治疗,为了达到再灌注的目的,可选择的治疗有术中局部使用IIb/IIIa受体抑制剂、球囊成型、支架植入。对于此类ICAS病变患者,目前Solumbra(支架联合抽吸导管取栓)技术是常用的标准取栓技术,但没有可靠证据证实此为最优方案。基于以上背景,我们中心提出SPACEMAN取栓技术,主要是针对ICAS病变导致急性大血管闭塞患者,各字母具体指代(支架+通过病变+抽吸+补救+微导丝+血管成型)。
SPACEMAN技术简介

①将支架展开,并将抽吸导管置于血栓上;
②抽吸导管穿过血栓置于支架远端;
③在不改变抽吸导管位置的情况下,负压吸引取出支架;
④微导丝在抽吸导管的引导下穿过闭塞病灶到达远端;
⑤抽吸导管撤回到闭塞近端后造影;
⑥球囊或支架血管成形术。
研究内容及结论
方式方法
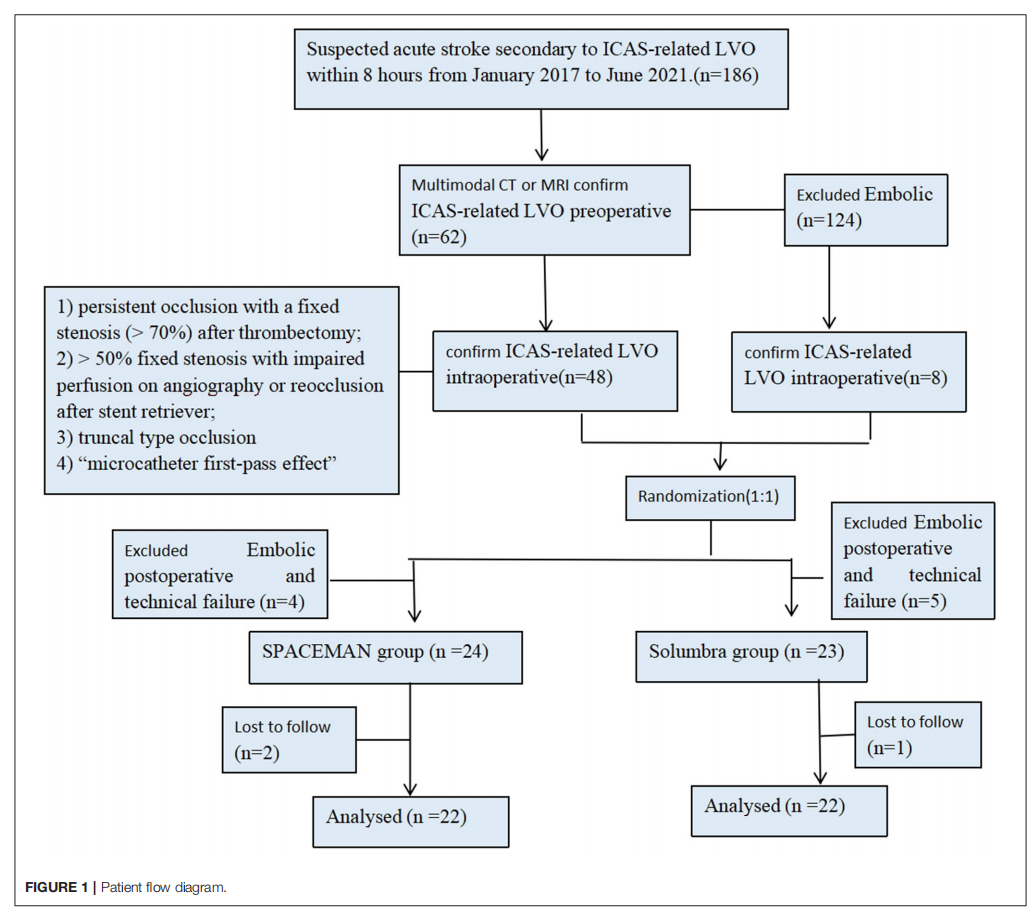
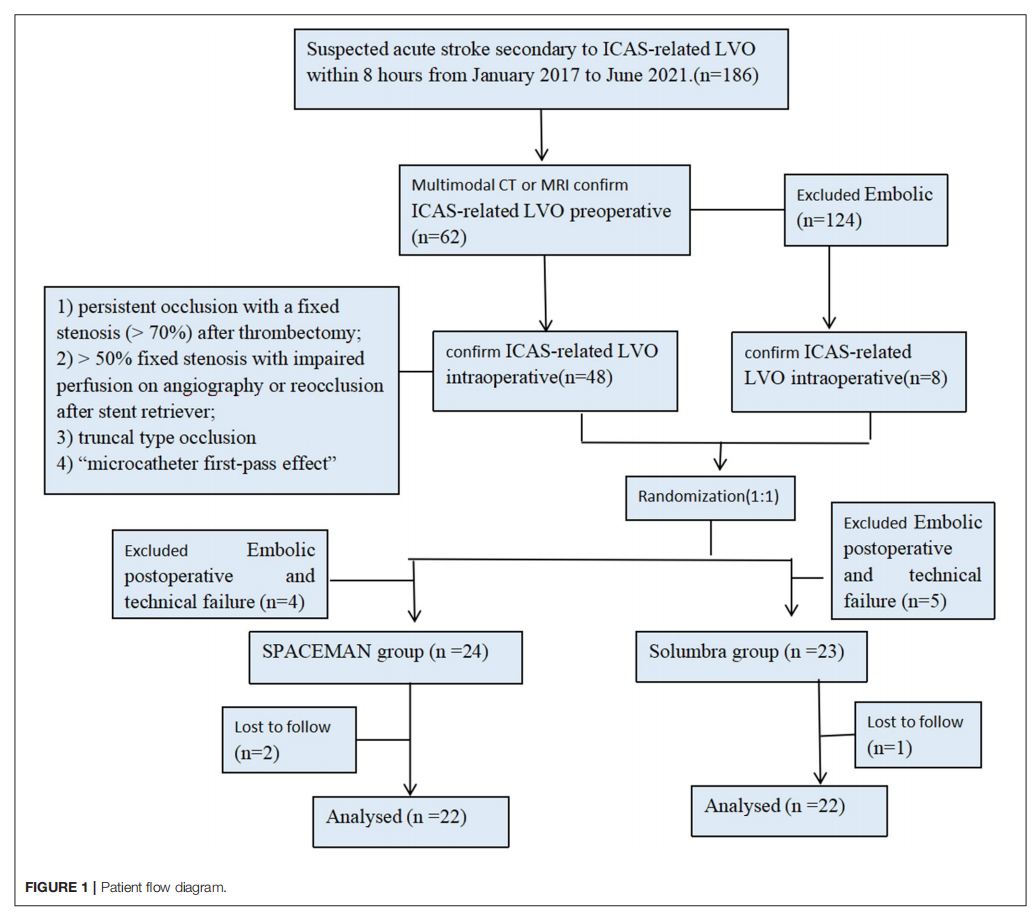
患者:入组从2017年1月致2021年6月鄂尔多斯市中心医院神经内科术前及术中确诊的由ICAS病变所致大血管闭塞共44例,采用随机分组为SPACEMANZ组(22例),Solumbra组(22例)。
结果显示(表1)
- 本院急性缺血性脑卒中中44例行机械取栓术(男32例,女12例;平均58.93±9.31年)。NIHSS平均评分为15.89±4.55分;
- 在年龄、性别、血管风险(高血压、糖尿病、高脂血症、房颤、冠心病、缺血性卒中和吸烟)、入院时NIHSS、DWI-ASPECTS评分、静脉溶栓或一般血管闭塞方面,组间无显着差异;
- ICAS二组间从症状出现到穿刺、补救性血管内治疗(球囊血管成形术和/或支架置入)的时间和栓塞率也相似;
- SPACEMAN组无技术相关并发症或栓塞发生。
- SPACEMAN组从股动脉入路到再通的平均时间短于Solumbra组(39.55±10.63 vs. 50.73±9.89 min, P = 0.001)。
结果显示(表2)
41例患者实现再灌注(再通率:93.18%)。在SPACEMAN组,95.45%的病例成功实现了再灌注(TICI 2b),而Solumbra组的再灌注成功率为90.91% (P = 1.000)。Solumbra组2例(9.09%)和SPACEMAN组1例(4.55%)发生颅内脑出血。90天mRS评分为2的患者数量spaceman组为13例(59.09%),Solumbra组为8例(36.36%)。spaceman组12例(54.55%)前循环病变获得良好预后(mRS: 0 2), Solumbra组8例(36.36%)。spaceman组4例(18.18%)后循环病变患者获得良好预后(mRS: 0 3), Solumbra组2例(9.09%)。SPACEMAN组前循环病变和后循环病变患者均有好转趋势,但组间差异无统计学意义。

本研究证明,对于由于ICAS病变所致的大血管闭塞性病变,这种结合抽吸导管、支架取栓及补救技术的新型取栓技术(SPACEMAN技术)是安全有效的。
典型病例展示
患者,男性,49岁,主因“左侧肢体麻木12小时,左侧肢体偏瘫6小时”入院。NIHSS: 10分。

①头部DWI:右侧大脑半球分水岭梗死;
②DSA:右侧MCA-M1段起始部闭塞;
③ SPACEMAN技术:
③(A)将抽吸导管放置在闭塞段附近,微导管证实真腔后释放支架。
③(B)手动负压下将抽吸导管置于支架远端,保持抽吸导管位置不变回撤支架。
③(C) 在抽吸导管引导下,将300 cm微导丝置于在MCA-M2段远端
③(D)抽吸导管撤回到闭塞近端后造影显示M1重度狭窄
③(E)在抽吸导管引导下将球囊扩张支架送至狭窄段扩张
③(F)血管成形术后DSA显示完全再通。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#前瞻性研究#
46
#前瞻性#
54
#SpA#
47
#EMA#
45
#取栓#
50
#ACE#
45