Neurology:神经结节病预后与病变定位相关,肿瘤坏死因子α拮抗剂优于单独使用皮质类固醇
2022-03-17 Naomi MedSci原创
脊髓结节病是一种罕见结节病表现。免疫疫抑制治疗的有神经后遗症在复发或进展率方面,脑膜定位的结节病与较差的预后相关;肿瘤坏死因子α拮抗剂与单独使用皮质类固醇相比显著降低;甲氨蝶呤比硫唑嘌呤更有效。
结节病是一种原因不明的慢性肉芽肿性疾病,可影响多个器官,主要是肺部和纵隔淋巴结,经常是皮肤、眼睛或肝脏。5%的患者可能累及神经系统,包括大约20%的病例涉及脊髓。
脊髓受累通常是结节病的首发症状,在15%-20%的患者中可能仅单个部位受累。结节病表现具有异质性,从类似多发性硬化症、视神经脊髓炎谱系障碍(NMOSD)的严重髓内脊髓炎,到与脑膜炎、脑膜脊髓炎相关的脊髓炎,这往往导致难以进行诊断性调查,并延误适当治疗的启动。根据观察性研究和专家意见的建议,脊髓结节病被认为是一种严重的局部性疾病,有很大的神经后遗症风险,需要长期的免疫抑制治疗。只有3项小规模研究试图确定预后因素,免疫抑制药物和肿瘤坏死因子α拮抗剂的各自效果需要调查。
近日,有研究人员对确诊的或可能的神经结节病合并脊髓受累的患者进行了全国性、多中心的回顾性研究。研究目标是通过比较未经治疗的患者或口服免疫抑制药物、肿瘤坏死因子α拮抗剂或环磷酰胺与单独使用皮质类固醇的患者的复发或进展率,来评估预后因素和免疫抑制治疗对疾病演变的疗效。
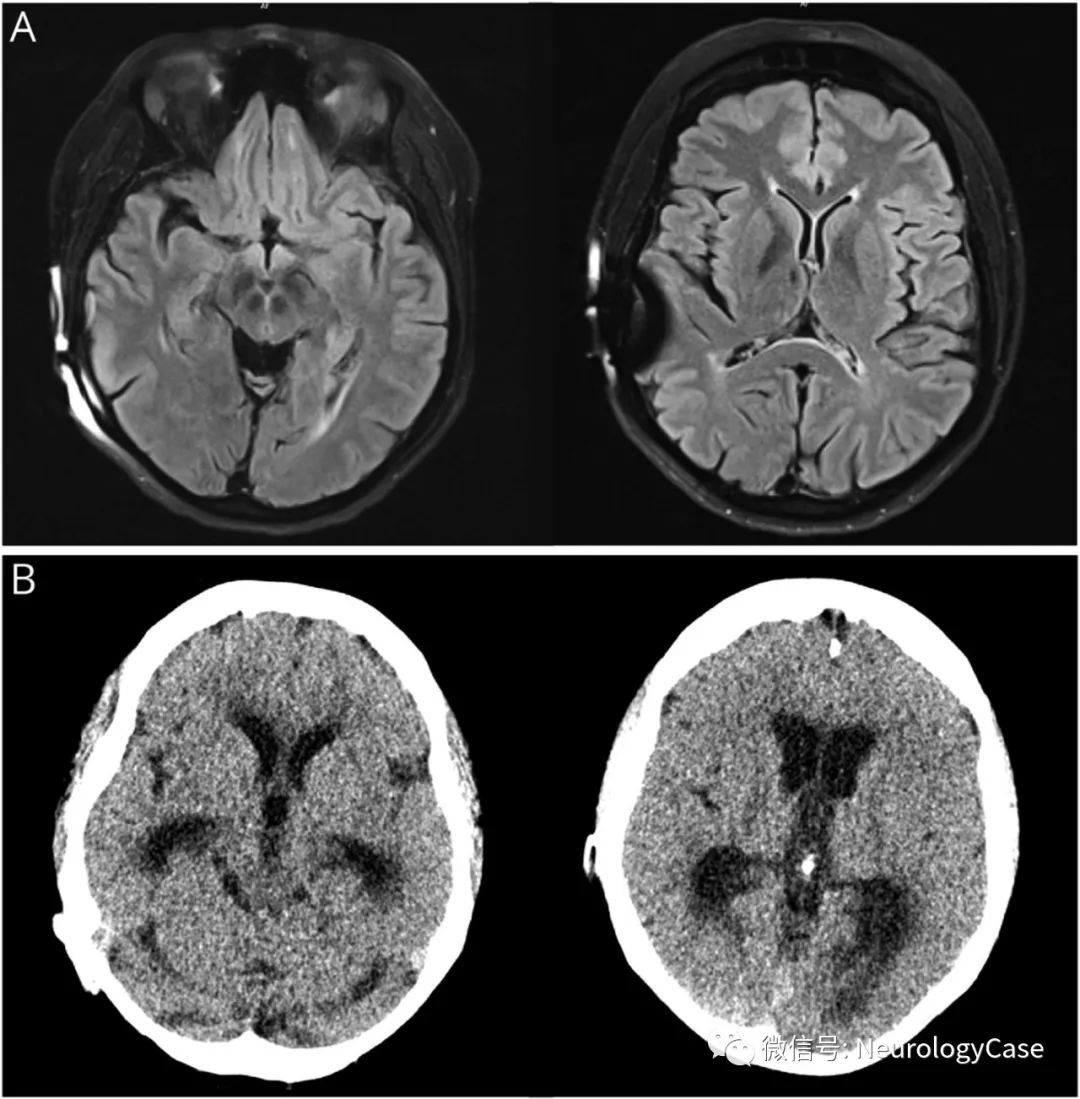
研究者对法国7个中心1995-2021年间随访的脊髓结节病患者进行了回顾性研究。根据神经结节病联合会共识组标准确定、可能或可能患有脊髓结节病,并经MRI证实脊髓受累的患者包括在内。用泊松模型分析复发或进展率,用线性模型分析初始Rankin评分,用Logistic模型分析随访期间Rankin评分的变化。
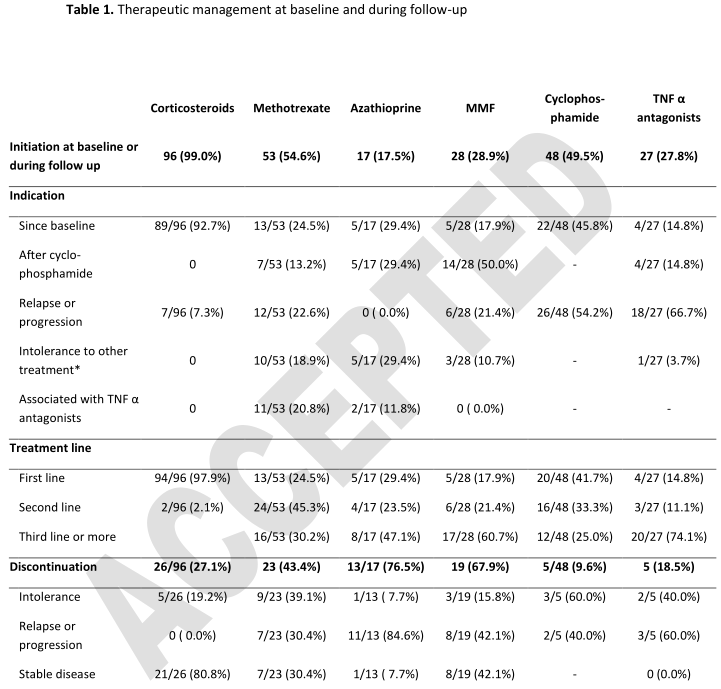
- 总共对97名患者进行了中位时间7.8年的随访。
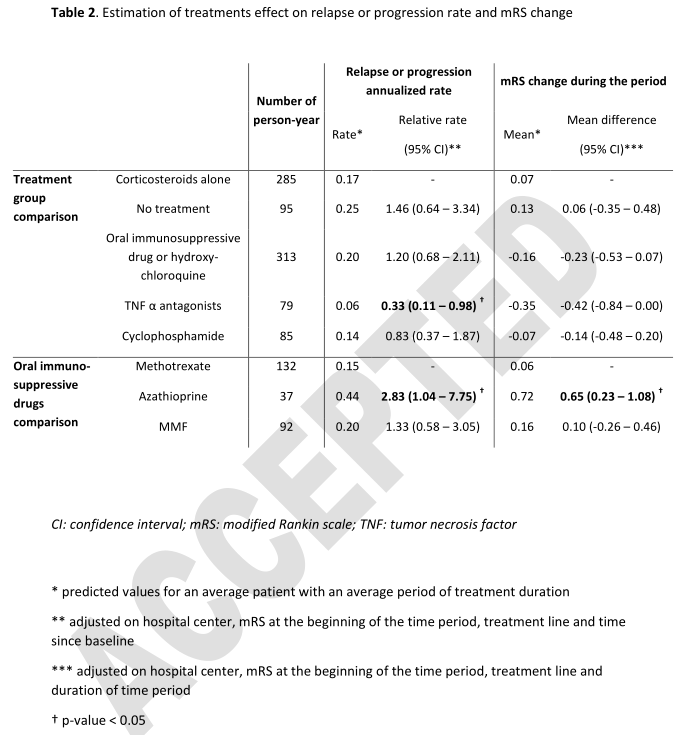
- 总体平均复发或进展率为0.17/人-年,并随着时间的推移而下降。最后一次就诊时,46例(47.4%)患者丧失了自主性(Rankin评分≥2)。
- 与复发或进展率显著相关的主要预后因素是脊髓MRI的Gd强化(相对比率[95%CI]:0.61[0.4,0.95])或脑膜受累(相对比率[95%CI]:2.05[1.31,3.19])和脑脊液分析的细胞计数(相对比率[95%CI]每1对数增加:1.16[1.01,1.33])。
- 复发或进展率与初始Rankin评分或EDSS没有显著相关性。
- 与单用糖皮质激素相比,肿瘤坏死因子α拮抗剂显著降低复发或进展率(相对率[95%CI]:0.33[0.11,0.98])。
- 在复发或进展率(相对率[95%CI]:2.83[1.04,7.75])和Rankin评分改变(平均差值[95%CI]:0.65[0.23,1.08])方面,硫唑嘌呤的疗效明显低于甲氨蝶呤。
在复发或进展率方面,脑膜定位的结节病与较差的预后相关;肿瘤坏死因子α拮抗剂与单独使用皮质类固醇相比显著降低;甲氨蝶呤比硫唑嘌呤更有效。
这项研究提供了IV类证据,证明在患有脊髓神经结节病的患者中,与单独使用皮质类固醇相比,肿瘤坏死因子α拮抗剂与降低复发或进展率有关,但其他治疗方法没有显著好处。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#神经结节病#
50
#Neurol#
46
#类固醇#
38
#坏死#
51
#肿瘤坏死因子#
51
#拮抗剂#
0