JACC:ACEI类药物对终末期心力衰竭的心肌Ang代谢的影响
2021-04-07 MedSci原创 MedSci原创
晚期心力衰竭(HF)是指HF患者即使接受了最大程度的循证治疗,仍持续出现影响日常生活的严重症状。
晚期心力衰竭(HF)是指HF患者即使接受了最大程度的循证治疗,仍持续出现影响日常生活的严重症状。晚期HF也称为“难治性”、“终末期”HF。患者的症状通常包括运动不耐受、非刻意的体重减轻、难治性容量超负荷、复发性室性心律失常,以及低血压和灌注不足的体征。
MAYO Clinic
血管紧张素,亦称血管收缩素、血管紧缩素、血管张力素,是一种寡肽类激素,是肾素-血管紧张素系统(RAS)的重要组成部分。血管紧张素能引起血管收缩,升高血压;促进肾上腺皮质释放醛固酮。它也具有很强的致渴作用。
目前治疗HF的药物中,很重要的一类为被称为“A”药的ACEI/ARB类——可减少血管紧张素Ⅱ的形成,从而降低小动脉和静脉阻力。由于ACEI对心脏、血管和肾脏等靶器官的多重效应,有研究表明它能延缓进行性心功能不全的进展,并在1-3年时使心血管死亡率降低约25%。
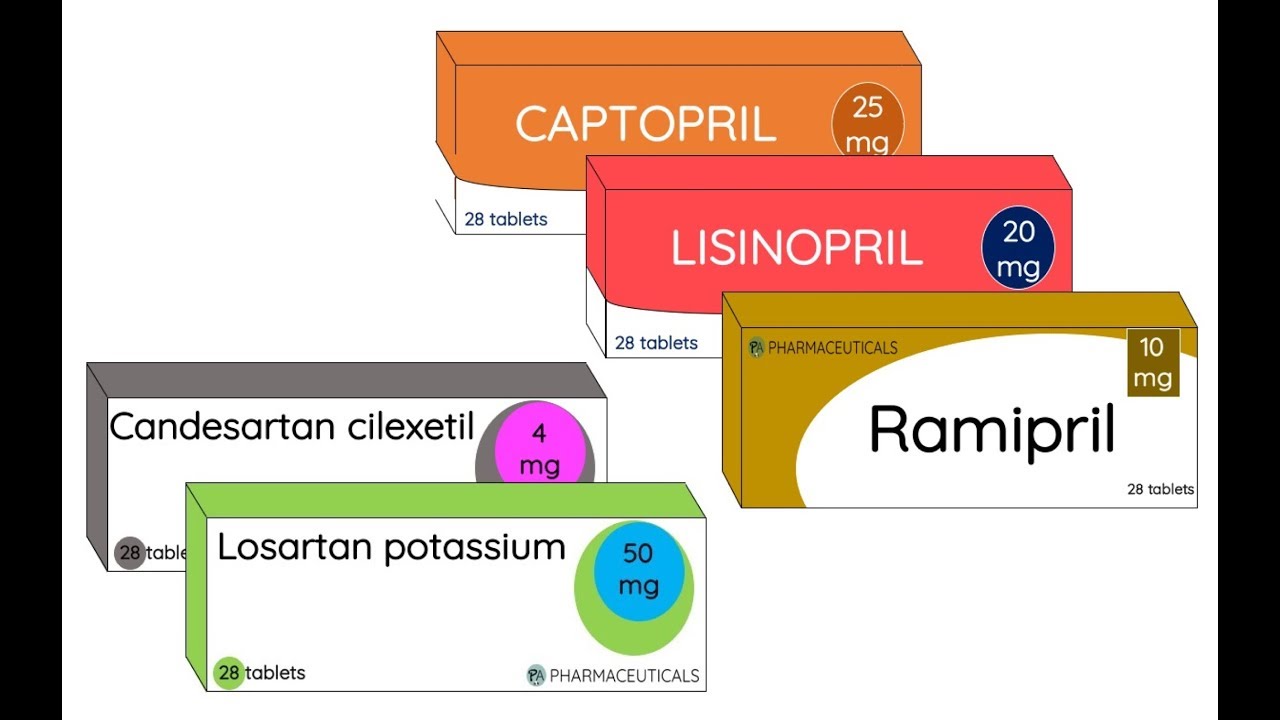
代表性的ACEI类药物
目前的研究认为,HF患者的心肌表现出适应性RAS系统,局部失衡可能会影响药物性RAS抑制的预期效果,而后者正是射血分数降低的心力衰竭(HFrEF)治疗的主要手段。那么,了解HF患者,尤其是终末期HF患者的血管紧张素代谢水平对使用ACEI类药物的精确治疗十分重要。
近期,来自奥地利维也纳大学医学院心血管领域的专家发表在《美国心脏病学会杂志》(JACC)上的最新研究就试图根据治疗情况,探讨人体心肌组织RAS对终末期心脏的调节作用。
研究人员纳入52名接受心脏移植的终末期HFrEF患者(无RAS抑制剂:n = 9;ACEI:n = 28;ARB:n = 8;ARNi:n = 7)。通过质谱法测定左心室样本中心肌血管紧张素代谢产物和参与关键血管紧张素肽血管紧张素1-8(AngII)和Ang1-7代谢的酶活性。
结果显示,AngII和Ang2-8(AngIII)是衰竭心脏中最主要的多肽,而其他代谢物,尤其是Ang1-7低于检测限度。接受ARB成分的患者的心脏AngII和AngIII水平显著升高。同时,心肌AngII浓度与循环AngII水平密切相关。
此外,研究人员观察到心肌RAS酶的调节与所使用的RAS抑制剂的类别无关。组织糜蛋白酶被认为是心脏AngII生成的主要酶,而AngII经脯氨酸羧肽酶代谢为Ang1-7,但不代谢为ACE2。
RAS系统相关肽的代谢和调节作用示意图
研究人员指出,心衰患者心脏中经典的RAS代谢物浓度较高,而AngIII可能是一种未被认识到的对心血管结构产生不利影响的介质。
综上,该研究强调了抑制循环AngII作用药物(ACEI)的重要性,同时也为旨在抑制心肌AngII/AngIII积累和作用的心脏组织特异性RAS药物提供了空间。
参考文献:
Myocardial Angiotensin Metabolism in End-Stage Heart Failure. J Am Coll Cardiol. 2021 Apr, 77 (14) 1731–1743
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#终末期#
30
#ACE#
30
#JACC#
31
受用
82
#ACC#
48