Blood:γ分泌酶抑制剂可增强BCMA靶向CAR T细胞疗法的功效
2019-10-01 MedSci MedSci原创
小分子γ分泌酶抑制剂可增加骨髓瘤细胞表面的BCMA表达量,进而增强CAR-T细胞的功效。
中心点:
小分子γ分泌酶抑制剂可增加骨髓瘤细胞表面的BCMA表达量,进而增强CAR-T细胞的功效
摘要:
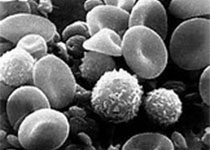
B细胞成熟抗原(BCMA)是嵌合抗原受体(CAR) T细胞治疗多发性骨髓瘤(MM)的有效靶点。虽然客观缓解率较好,但大多数患者会复发;肿瘤细胞亚群上的低BCMA水平被认为是一种可能的逃逸机制。
BCMA被无处不在的多亚单位的γ分泌酶复合物从肿瘤细胞表面主动裂解掉,导致在肿瘤细胞上用于CAR-T细胞识别的配体密度降低,并释放可溶性BCMA (sBCMA)片段,抑制CAR-T细胞功能。足量的sBCMA可在MM患者骨髓中积累,抑制CAR-T细胞识别肿瘤细胞,并可能潜在限制BCMA介导的适应性T细胞疗法的疗效。
用小分子γ-分泌酶抑制剂(GSIs)阻断BCMA清除是否可增强BCMA靶向CAR-T细胞疗法的疗效?研究人员对此进行探究。研究人员发现用GSIs处理骨髓瘤细胞系和患者的肿瘤样本均可以一种剂量依赖性的方式显著增加肿瘤细胞表面的BCMA水平,同时降低sBCMA浓度,提高CAT-T细胞对体外肿瘤细胞的识别。GSI治疗NOD/SCID/γc-/-小鼠的MM肿瘤可增加肿瘤细胞上的BCMA表达,减少外周血中的sBCMA,提高BCMA靶向CAR-T细胞疗法的抗肿瘤效应。最重要的是,给MM患者短疗程使用GSI可显著增加BCMA+肿瘤细胞的比例,和体内BCMA在细胞表面的表达水平。
原始出处:
Margot J. Pont, et al.γ-secretase inhibition increases efficacy of BCMA-specific chimeric antigen receptor T cells in multiple myeloma.Blood 2019 :blood.2019000050; doi: https://doi.org/10.1182/blood.2019000050
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抑制剂#
36
#分泌#
42
#BCMA#
44
#T细胞疗法#
38
#分泌酶#
38
很好的学习机会
73
好好好好好好
65
学习了
77