Pediatrics:早产儿拔管后的吸氧方式对比
2021-09-10 从医路漫漫 MedSci原创
比较早产儿拔管后高流量鼻插管(HFNC)与鼻持续正压通气(NCPAP)或鼻间歇正压通气(NIPPV)的疗效和安全性。
目的:比较早产儿拔管后高流量鼻插管(HFNC)与鼻持续正压通气(NCPAP)或鼻间歇正压通气(NIPPV)的疗效和安全性。
方法:在6个三级医院的新生儿重症监护室进行前瞻性、随机、非劣效性试验。纳入34周出生、拔管后需要无创通气的婴儿。使用HFNC的婴儿分配到HFNC组,使用NCPAP或NIPPV的婴儿分配到NCPAP/NIPPV组。主要结果是拔管后7天内治疗失败。然后我们检查了HFNC治疗失败的临床方面原因。
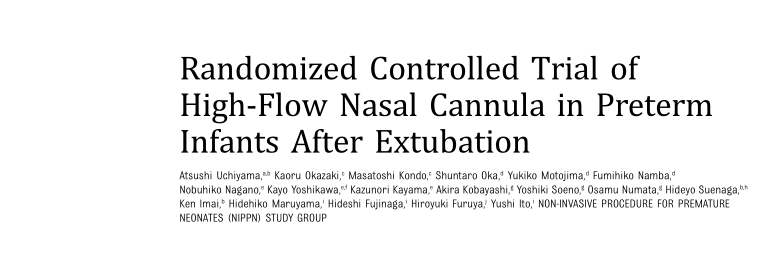
结果:176例和196例婴儿分别被分为HFNC组和NCPAP/NIPPV组。HFNC组治疗失败率显著高于NCPAP/NIPPV组,其中54例(31%)患儿治疗失败,NCPAP/NIPPV组31例(16%)患儿治疗失败(风险差异,14.9个百分点;95%置信区间,6.2-23.2)。组织学性绒毛膜羊膜炎(P=0 .02)、经治疗的动脉导管未闭(P=0 .001)和治疗开始时的校正胎龄(P= 0.007)是HFNC治疗失败的独立危险因素。
表 拔管后HFNC治疗失败的相关因素
结论:在早产儿拔管后,HFNC的治疗失败率明显高于NCPAP或NIPPV。与HFNC治疗失败相关的独立因素是:组织性绒毛膜羊膜炎、经治疗的动脉导管未闭和治疗开始时较小的校正胎龄
原文出处
Uchiyama A, Okazaki K, Kondo M, Randomized Controlled Trial of High-Flow Nasal Cannula in Preterm Infants After Extubation.Pediatrics 2020 12;146(6)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Pediatric#
44
#PE#
34
#DIA#
42
#拔管#
35
已学习
53