同济医院开设白血病停药门诊
2017-05-17 佚名 健康报
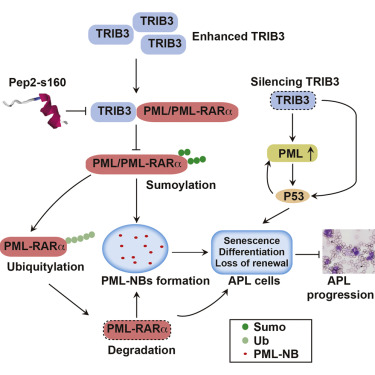
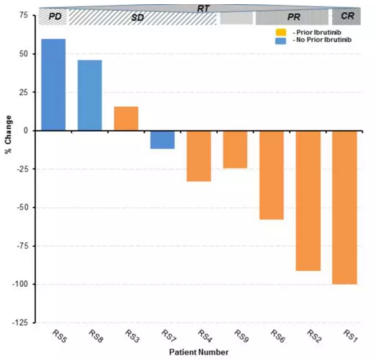
尽管靶向药物治疗慢性粒细胞白血病效果较好,但长期的药费给不少家庭带来沉重负担。近日,华中科技大学同济医学院附属同济医院开设停药门诊,有望帮助慢性粒细胞白血病患者实现停止服药。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#同济医院#
28
#停药#
35
好文章学习了
67
谢谢分享
62
学习了,谢谢分享
67
太棒了,这样减少了患者的经济负担
48
签到学习了很多。
64