Radiology:腹部CT扫描偶然发现的骨硬化性病变是否曾经困扰过你?
2021-06-10 shaosai MedSci原创
在临床上,骨硬化性病变常于腹部CT检查偶然发现。明确骨硬化性病变是骨岛还是成骨性骨转移瘤是决定进一步治疗方案的关键。骨岛没有临床意义,且无症状的骨岛不需要治疗。然而若为成骨性骨转移瘤,患者的治疗方案和
 在临床上,骨硬化性病变常于腹部CT检查偶然发现。明确骨硬化性病变是骨岛还是成骨性骨转移瘤是决定进一步治疗方案的关键。骨岛没有临床意义,且无症状的骨岛不需要治疗。然而若为成骨性骨转移瘤,患者的治疗方案和预后会发生极大改变。
在临床上,骨硬化性病变常于腹部CT检查偶然发现。明确骨硬化性病变是骨岛还是成骨性骨转移瘤是决定进一步治疗方案的关键。骨岛没有临床意义,且无症状的骨岛不需要治疗。然而若为成骨性骨转移瘤,患者的治疗方案和预后会发生极大改变。
骨岛的典型CT表现为针状边缘、骨小梁增粗且无如骨破坏、骨膜反应或软组织受累等恶性特征。然而,很多骨岛的影像学表现并不典型,部分骨岛甚至在骨显像或PET/CT上显示为热摄取,导致骨岛与恶性病变的鉴别极具挑战。
放射组学可从临床图像中提取和分析出无法通过肉眼检查评估的定量信息。放射组学提取和分析的信息反可映肿瘤的病理生理学状态。在肌肉骨骼放射学中,放射组学已被用于良、恶性病变的鉴别、预测肿瘤分级、患者预后和治疗反应。
近日,发表在Radiology杂志的一项研究建立一个基于CT放射组学的机器学习模型,并评估了其对骨岛和成骨性骨转移瘤的鉴别诊断性能,为临床提供了一个可靠的、快速诊断骨硬化性病变的影像学手段。
本项回顾性研究纳入了2015年至2019年期间在两个不同机构中接受腹部增强CT检查并诊断为骨岛或成骨性骨转移瘤的患者:机构1为训练集,机构2为外部测试集。提取放射组学特征。选取10个特征建立随机森林( RF)模型,并进行10倍交叉验证。在测试阶段,使用外部测试集测试RF模型。三名放射科医生对测试集中的CT图像进行了审阅。计算模型和三位放射科医生的敏感性、特异性、准确性和受者工作特征曲线下面积(AUC),并对放射组学模型和放射科医师的AUC进行比较。
训练集177例患者(89例骨岛,88例骨转移瘤;平均年龄66岁±12岁(标准差),111名男性),测试集64名(23名骨岛,41名骨转移瘤;平均年龄69岁±14岁,59名男性)。提取放射组学特征(n = 1218)。通过10倍交叉验证,RF模型的平均AUC为0.89(敏感性,85%[88例患者中的75例];特异性为82%[89例患者中的73例];准确性为84%[177例患者中的148例])。在测试集中,训练后的RF模型的AUC为0.96(敏感性,80%[41例患者中的33例];特异性,96%[23例患者中的22例];准确率为86%[64例患者中55例])。三个阅读者的AUC分别为0.95 (95% CI: 0.90, 1.00)、0.96 (95% CI: 0.90, 1.00)和0.88 (95% CI: 0.80, 0.96)。放射组学模型的AUC仅显著高于阅读者3(0.96 vs 0.88;P = 03)。
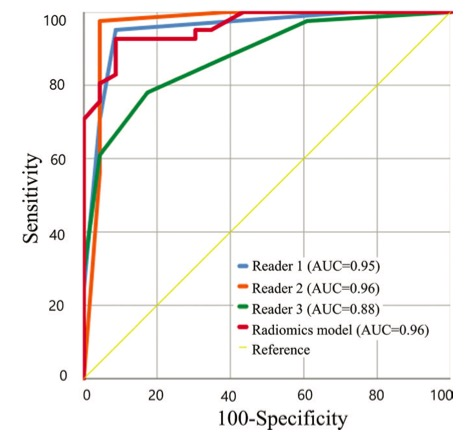
图1 该图显示了基于放射组学的随机森林模型以及外部测试集中区分骨岛和成骨性骨转移瘤的三个阅读者的受试者工作特征曲线。放射组学模型的受试者工作特征曲线下面积(AUC)高于阅读者 3(0.96 vs 0.88;P = .03),且与阅读者1、2相当(P = .81、P = .88)。

表1 放射组学模型的诊断性能以及外部测试集中与衰减或形状相关的特征。
本研究表明,基于CT放射组学的随机森林模型可以用于骨岛和成骨性骨转移瘤的鉴别。同时,与经验较少的放射科医生相比,放射组学模型的诊断性能更佳,并可与经验丰富的放射科医生相媲美。本研究为临床正确处理偶然发现的骨硬化性病变及提高放射科医生的诊断信心提供了技术支持。
原文出处:
Ji Hyun Hong,Joon-Yong Jung,Aram Jo,et al.Development and Validation of a Radiomics Model for Differentiating Bone Islands and Osteoblastic Bone Metastases at Abdominal CT.DOI:10.1148/radiol.2021203783
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腹部CT#
30
学习了
61
#硬化性#
31
#CT扫描#
40
学习了
69