Eur Radiol: 关于多系统萎缩,仅靠“十字面包征”进行诊断是否为时太晚?!
2021-01-06 shaosai MedSci原创
在神经影像上,“十字面包”征是非常典型的神经退行性变的影像学征象,你知道是哪种疾病的典型MRI表现吗? 作为神经科或影像科的医生,通过上述征象进行多系统萎缩(MSA)的诊断就够了吗?
在神经影像上,“十字面包”征是非常典型的神经退行性变的影像学征象,你知道是哪种疾病的典型MRI表现吗?
作为神经科或影像科的医生,通过上述征象进行多系统萎缩(MSA)的诊断就够了吗?
或许知道这些,远远不够!——因为出现这些征象时,现代医疗水平对患者的生存质量及生存期的改变能力微乎其微,且存的对症治疗方案往往差强人意,尚无有效的神经保护性治疗措施来改善及延缓病情的发展。
如何能够进行早期的准确诊断及鉴别诊断、找到病情进展的征象对评估患者预后及为后续临床研究评价才是让患者获益的最基本的不二法宝!
MSA是一种进行性神经退行性疾病,以不自主运动、小脑共济失调、震颤麻痹及锥体束征候为主要特点的疾病,其发病率约占1.9%-4.9%。MSA是一种不可治愈性疾病,通常在出现临床症状后7-9年死亡。MSA共有两个临床亚型:以小脑共济失调为主的MSA(MSA-C)和以震颤麻痹为主的MSA(MSA-P)。
目前对于MSA的诊断尚无有效的评判方法,尤其是在疾病早期。如何能够早期识别MSA高危人群以及定量评价MSA严重程度是非常迫切的。
近日,Eur Radiol上发表的一篇名为Magnetic resonance T1w/T2w ratio in the middle cerebellar peduncle might be a sensitive biomarker for multiple system atrophy的论文利用髓磷脂敏感的MRI对比剂以及标准化的T1加权/ T2加权(sT1w / T2w)比值来定量评估多系统萎缩症小脑亚型(MSA-C)患者小脑中脚(MCP)的早期变化。

该研究纳入了28名MSA-C患者,包括在发病2年内(早期MSA-C)的17名MSA-C患者和28名健康对照者。使用3T MR进行T1w和T2w图像采集。使用SPM12分析了MCP感兴趣区中sT1w / T2w比值大小;评价了利用MCP sT1w / T2w比值识别MSA-C、早期MSA-C亚组及健康志愿者的鉴别诊断能力;同时将MCP sT1w / T2w比值与其他临床参数进行相关性分析(ICARS量表等)。
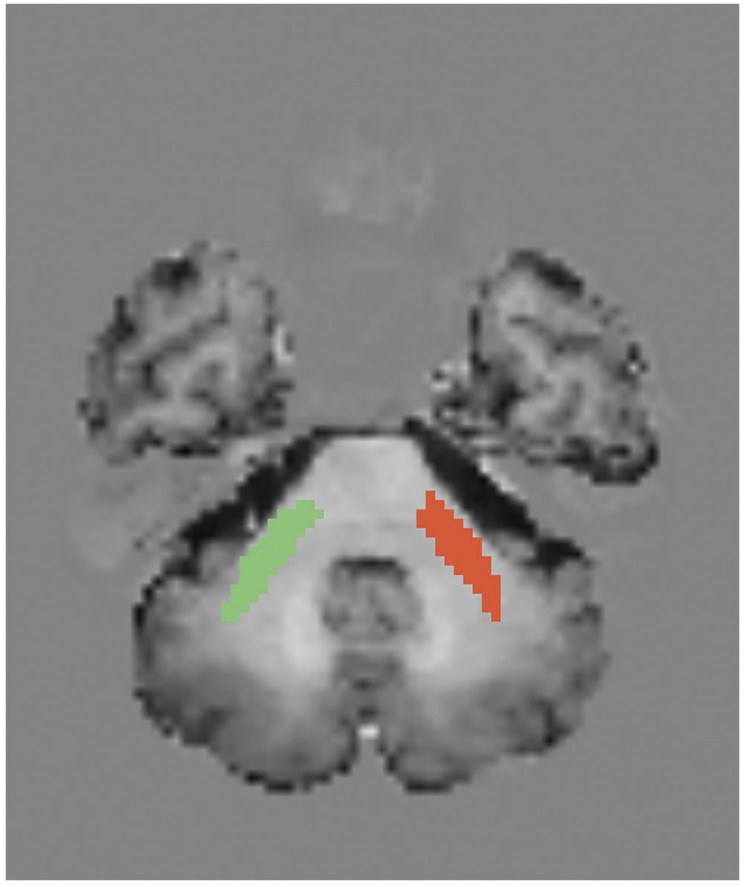
图1.双侧小脑中脚感兴趣勾画示意图
研究分析得出:所有MSA-C患者(p <0.001)及17例早期(p <0.001)MSA-C患者的MCPsT1w / T2w比值均显着低于健康对照组。MCP sT1w / T2w比值在区分MSA-C与对照组上具有很高的灵敏度(96%)和特异性(100%)(曲线下面积= 0.99);即使在早期MSA-C组(曲线下面积= 0.99)该指标也具有很高的诊断效能(灵敏度= 94%,特异性= 100%)。此外,在早期MSA-C组中,MCP sT1w / T2w比值与ICARS评分有高度相关性。
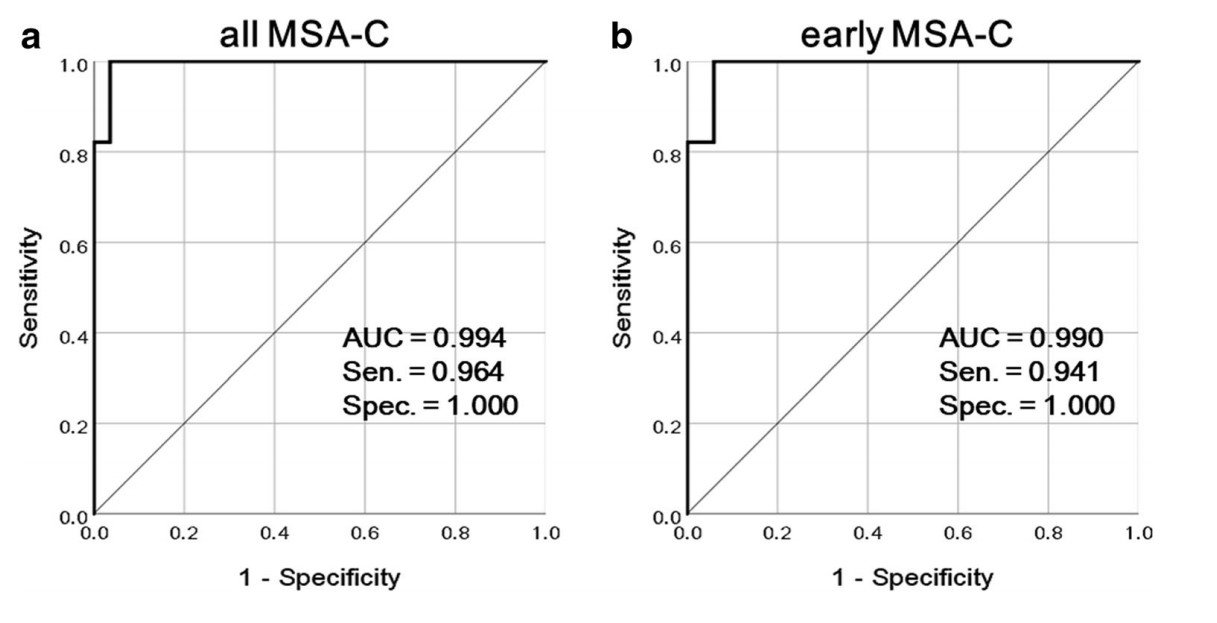
图2. MCP sT1w / T2w比值对诊断所有MSA-C及早期MSA-C的诊断效能
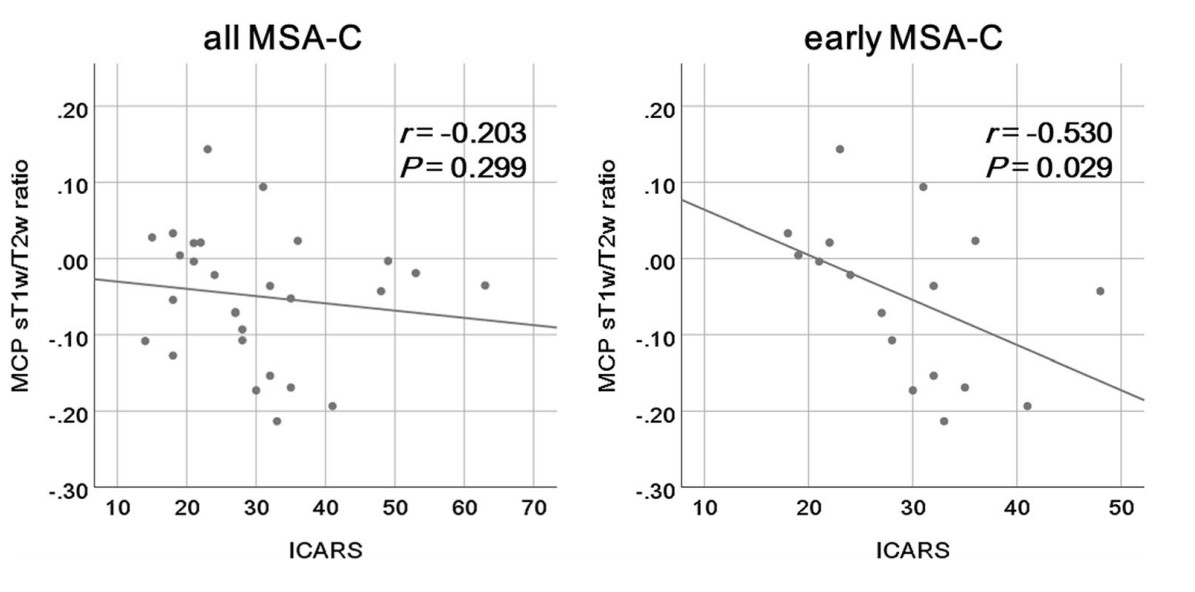
图3. MCP sT1w / T2w比值与ICARS评分的相关性分析
该研究结果表明sT1w / T2w比值能够早期识别MCP中MSA-C相关变化,也许可以作为发现及诊断MSA-C的敏感的生物标志物。
写在后面:
影像学的诊断最终目的是服务与临床。当影像学诊断对临床决策或者说临床获益无济于事时,它也是无价值的。该研究结果能够早期地诊断或排除多系统萎缩的存在,这无疑对及时的临床监管是非常重要;同时,定量的评价,能够有效地用数字说话来评估预后!
原始出处:
Atsuhiko Sugiyama,Hajime Yokota,Shigeki Hirano,et al. Magnetic resonance T1w/T2w ratio in the middle cerebellar peduncle might be a sensitive biomarker for multiple system atrophy. PMID:33241514DOI:10.1007/s00330-020-07521-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


.jpg)









#萎缩#
34
很有意义,学习了
75
#多系统萎缩#
35
有必要
86
学习了!
86