JAMA:动摇欧美指南!湘雅医生团队分析近9万患者数据首次发现,用曲马多治骨关节炎与患者全因死亡风险增加104%相关
2019-03-26 奇点糕 奇点网
常追剧的小伙伴对这样的场景肯定不陌生:久经沙场的老将军雄风不在,身上的旧伤总是会疼痛难忍。
常追剧的小伙伴对这样的场景肯定不陌生:久经沙场的老将军雄风不在,身上的旧伤总是会疼痛难忍。
根据奇点糕的猜测,这很有可能是关节炎。由于长期的关节劳损、外伤或其他原因,关节及其周围组织发热、肿痛,整个人陷入无尽的疼痛折磨中。
遗憾的是,时至今日,我们对于关节炎还没有很好的治疗方法,尤其是其中的骨关节炎,主要的治疗目标,也只能是,缓解疼痛,延缓疾病进展,矫正畸形,改善或恢复关节功能,改善患者的生活质量。
由于镇痛药物的特殊性,药物毒性的研究变得至关重要。但是,即使小心再小心,也总有令人大吃一惊、无比后怕的事情发生。
就比如说近日发表在JAMA上的一篇文章,根据中南大学湘雅医院骨科雷光华教授团队与哈佛大学张余庆教授团队的研究成果,使用骨关节炎一线镇痛药物曲马多,与其他非甾体抗炎药物相比,跟患者全因死亡风险提高70%-104%有关!
雷光华教授(左)张余庆教授(右)
随着世界卫生组织(WHO)“骨与关节十年”活动的启动,骨骼疾病愈加受到重视。
骨关节炎(OA)是骨骼疾病中的一种,在75岁以上的人群中,患病率接近80%。其造成的关节肿痛、骨质增生和活动受限严重降低了患者的生活质量,影响正常生活。
在我国,60岁以上人口已经超过了一亿,而据估计,其中骨关节炎患者就有5000万。随着人口老龄化,这一问题必将更加突出,有效治疗骨关节炎成为重大的公共卫生学问题。
但是,由于骨关节炎的病因众多,并没有很好的方法将其根治,科学家们也只能退而求其次,控制骨关节炎引起的疼痛,力求不影响患者的正常生活。
阿片类药物的止痛效果良好,可以应对中度到重度的疼痛。但是由于它可以和中枢神经特异性受体相互作用,成瘾风险也十分高,还有可能造成呼吸抑制。
非甾体抗炎药物可以说是消炎止痛的一把好手,但是依然有不可避免的副作用,比如胃肠道的不良反应,还会增加心血管疾病风险。
与前两者相比,曲马多的优势十分明显,它不像阿片类药物有那么大的成瘾风险,对于胃肠道和心血管的反应也更加温和。
由此,美国骨科医师学会指南强烈推荐曲马多或非甾体抗炎药物治疗膝关节骨性关节炎,美国风湿病学会更是将曲马多写进指南(2012),有条件地推荐曲马多和非甾体抗炎药物作为膝关节骨性关节炎患者的一线治疗药物。在美国,使用曲马多治疗膝关节骨性关节炎的处方率从2003年的5%增加到了2009年的10%。
然而,曲马多并不是无懈可击。它是一种弱阿片受体激动剂,可以激活阿片受体,可能会对神经系统产生不利影响,增加死亡率。关于曲马多对骨关节炎患者全因死亡风险影响的研究还不甚完整,所以,雷光华教授和张余庆教授进行了这个研究。
患者数据来自英国普通诊所的电子医疗记录数据库(THIN),包括在2000年1月至2015年12月期间就诊、年龄在50岁及以上、有骨关节炎病史的88902名患者,有癌症病史或阿片类药物使用障碍的患者被排除。
这些患者接受曲马多或其他镇痛药物的治疗,包括萘普生或双氯芬酸(常用的非选择性非甾体抗炎药)、塞来昔布或依托考昔(环氧酶2抑制剂),还有可待因(常用弱阿片类药物),统计用药一年内的死亡人数。
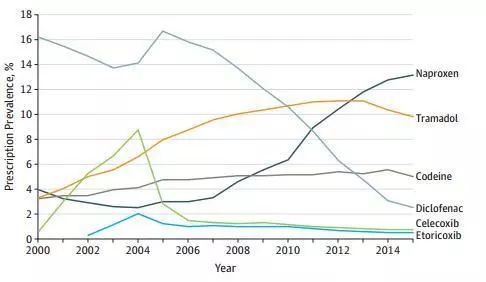
曲马多在英国骨关节炎患者中处方率较高(黄色)
统计数据说明,曲马多真不愧是被强烈推荐的药物,处方率从2000年的3.4%上升到2013年的11.1%,虽然之后有所下降,但是依然有9.8%(2015年)。本次研究中使用曲马多的英国患者多达44451名,占了总样本量的一半。
根据分析,曲马多和可待因同属弱阿片类药物,平均治疗时间相似,全因死亡风险也没多大差别。
但是和其他药物相比,曲马多的数据实在是让人出了一身冷汗。
虽然治疗时间的角度来看,曲马多是占据优势的,平均治疗时间仅为22天(5-67天),而其他药物都在24天-31天左右。

曲马多组(黄色)和萘普生组患者(蓝色)的全因死亡率
全因死亡风险统计结果却让人心惊。不论是和谁相比,曲马多组患者的全因死亡风险都远远领跑,分别比萘普生组全因死亡风险高71%,比双氯芬酸组全因死亡风险高88%,比塞来昔布组全因死亡风险高70%,比依托考昔组全因死亡风险高104%!
同时,曲马多组患者心血管、胃肠道、感染、癌症和呼吸系统疾病的死亡风险都要高于非甾体抗炎药物组。
对于曲马多的这种表现,研究人员是有一定的心理准备的。因为曲马多本身可能会增加低血糖、骨折或者跌倒的风险,这些都会增加老年人的死亡风险;如果服用曲马多的患者饮酒或者服用了其他中枢神经系统抑制剂,也有可能导致致命的呼吸抑制。
更何况,在消化性溃疡穿孔的治疗过程中,使用曲马多的患者,死亡风险也要高于使用非甾体抗炎药的患者。
但是,本次的研究依然存在一些局限性,比如有16.4%-29.7%的死亡原因无法确定,不能完全评估曲马多与死亡风险的关系,而且使用曲马多的患者大多年龄较大,BMI较高,本身死亡风险较高等。
所以,研究人员表示,还需要进一步的研究来确定曲马多与骨关节炎患者升高的全因死亡风险是否具有因果关系。
对于我国骨关节炎患者而言,目前指南推荐的首选用药还是非甾体抗炎药。所以大家也不用过度担心,选择更合理的生活方式,争取将关节炎扼杀在摇篮里。
但无论如何,研究结果都让人警醒,使临床医生在用药时更慎重地考虑曲马多的风险和受益,甚至可能会对美国指南产生影响,也对我国后续指南的制定有一定的指导意义。
总之,莫慌,等结果。
原始出处:Chao Zeng, MD, Maureen Dubreuil, MD, MSc Marc R. LaRochelle, et al. Association of Tramadol With All-Cause Mortality Among Patients With Osteoarthritis. JAMA. March 12, 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者数据#
28
#骨关节#
21
#全因死亡风险#
21
#死亡风险#
30
#关节炎#
30
#曲马多#
33
#湘雅#
30
值得学习,谢谢分享。
49
学习谢谢分享
56