第十七届中国介入心脏病学大会(CIT2019)|王海昌:ACS急诊PCI术中并发症紧急处理技巧
2019-03-29 Gill MedSci原创
ACS急诊PCI术中并发症紧急处理技巧第十七届中国介入心脏病学大会(CIT2019)将于2019年3月28日~31日在北京国家会议中心召开。来自第四军医大学唐都医院的王海昌教授在大会分享了急诊PCI手术中可能遇到的问题及应对策略。STEM急诊PCI常见并发症包括:1.心源性休克2.心律失常3.血栓脱落4.慢血流、无复流5.心脏破裂6.目标漂移(多支血管病变)等等首先需要明确,急诊PCI手术目标为开
第十七届中国介入心脏病学大会(CIT2019)于2019年3月28日~31日在北京国家会议中心召开,目前正在火热进行中。会中将发布CIT年度最新临床试验、众多国际知名学术的联合学术活动;内容涉及冠心病、瓣膜和结构性心脏病、外周血管病、心律失常、高血压 和心力衰竭及相关药物治疗诸领域的最新进展学术报告。
来自第四军医大学唐都医院的王海昌教授在大会分享了急诊PCI手术中可能遇到的问题及应对策略。
首先需要明确,急诊PCI手术目标为开通血管,其唯一目标就是恢复靶变血管三级血流!术前谈话中必须和患者及家属明确介入手术的目的和风险,告知非单纯等同于救命,尽量规避术后纠纷风险。
- AMI合并心源性休克介入治疗
AMI合并心源性休克是急诊中最棘手的类型。对于可开通的血管应尽力开通,并且不受时间限制,即使在心梗发生数小时后也应该尽量行介入治疗。
例:一例下壁急性心梗患者,已放置IABP导管,冠脉造影提示:除左主干严重狭窄外,右冠脉三段还存在严重栓塞;那么此时行PCI治疗应选择开通左侧冠脉还是右侧冠脉呢?

最后对患者进行了右侧冠脉介入治疗,因为右侧冠脉负责前降支、回旋支、左冠脉供血,但术中开通血管需十分谨慎,若开通右冠脉开通失败,则导致全冠脉无灌注血流,死亡风险巨大。
- AMI合并心律失常
AMI 介入术中可突发各种类型心律失常。
例:此为一例急性下壁ST段抬高型心梗在PCI术中突发室性心动过速的病例。
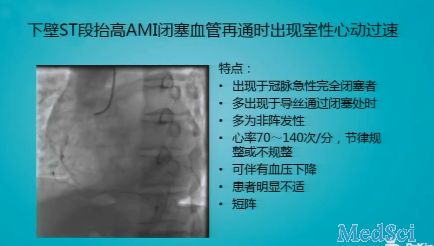
这种情况多数出现于冠脉急性完全闭塞者,多在导丝通过闭塞处时出现。心律失常多为阵发性,心率在70-140bpm,节律可规整或不规整,并伴有血压下降和不适感。
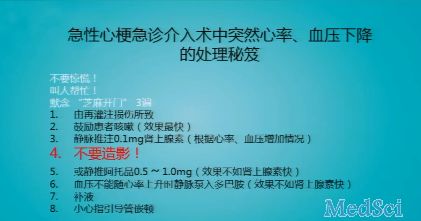
例:一例下壁ST段抬高AMI在PCI术中突发心率、血压下降,并伴有极度不适和躁动。

面对这种情况,记住一定要冷静。这多数是因为冠脉恢复再灌注时诱发的心律失常,切记不要注射造影剂!可嘱患者咳嗽,判断其意识状况并让血流迅速返回至脑部,根据心率、血压情况适当静脉注射肾上腺素或阿托品,当血压不能随心率上升恢复时,可静脉泵入多巴胺,下壁梗死时适当补充液体也十分有效。
面对此类病例可以牢记以下口诀应对处理:
- AMI合并血栓脱落
前降支伴血栓也可表现为心率慢、血压低,处理时应谨慎小心,若术中处理时导致血栓脱落至回旋支则十分危险!
AMI合并慢血流
例:一例急性AMI在PCI术中突发心率、血压为零,冠脉造影显示无血流灌注。
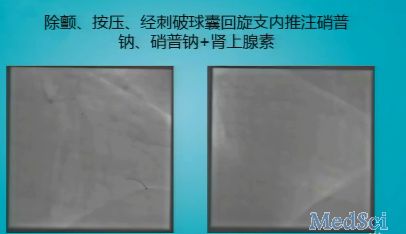
抢救过程中将刺破球囊置入回旋支,并向其中注入硝普钠,静脉推入硝普纳+肾上腺素,并反复除颤、胸外按压,心率血压恢复后,回旋支远端放置支架,支架植入后切勿造影!应大量注入硝普钠待血流恢复后再行造影。
- AMI合并心脏破裂
临床上AMI术中出现心脏破裂较为少见。
例:一例下壁AMI患者血管再通过程中突发心脏破裂,造影显示心脏影与心包影之间明显间隔。

在造影过程中,如果发现心脏局部染色不均特变明显,一定要警惕心脏破裂发生,完善心脏彩超检查。
- AMI合并目标漂移
例:一例下壁亚急性心梗,前降支中段严重狭窄。
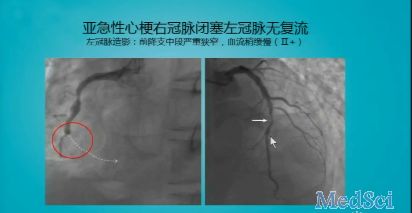
行右冠脉开通后三级血流仍无法恢复,于是在左侧冠脉狭窄处放置支架,随后病人发生慢血流;予以抢救后恢复。本例原本为右冠脉闭塞导致的亚急性心梗,当术中开通右侧无效后予以左侧支架置入,结果诱发了左侧冠脉慢血流。
PCI术中可能突发各种情况,只有积累足够的临床经验后方可自如应对,不过最重要的还是保持冷静,牢记恢复血流再灌注的原则后谨慎处理。
本次大会更多精彩内容,敬请期待梅斯后续报道。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PCI术#
30
#急诊PCI#
32
#介入心脏病学#
27
#紧急处理#
30
#心脏病学#
34
#并发#
23
#CIT#
21
#ACS#
23
#紧急#
24
值得学习,谢谢分享。
61