Science:手术等无菌损伤中腹腔粘连形成与原始的GATA6巨噬细胞有关
2021-03-06 MedSci原创 MedSci原创
腹腔内的疤痕称为粘连,是在炎症或手术后形成的。它们会造成机体慢性疼痛和消化问题,导致女性不孕,甚至可能危及生命,如肠梗阻。
腹腔内的疤痕称为粘连,是在炎症或手术后形成的。它们会造成机体慢性疼痛和消化问题,导致女性不孕,甚至可能危及生命,如肠梗阻。如果出现粘连就必须再次手术,腹腔粘连也使后续的手术干预更加困难,这给患者带来了巨大的痛苦,也给医疗保健系统带来了巨大的财政负担。仅在美国,腹部粘连每年的医疗费用就高达23亿美元。

pixabay.com
目前关于粘连形成的原因还不完全了解,也没有治疗方法。“由于这种疾病很大程度上在研究中被忽视了,所以我们在伯尔尼启动了这个项目,以了解更多关于粘连的发展,”这项研究的合著者Daniel Candinas说到。已经有研究者猜测巨噬细胞在粘连形成中起决定性作用。来自Inselspital内脏外科和医学系以及伯尔尼大学生物医学研究部(DBMR)的Joel Zindel和Daniel Candinas证实了这一点。
随后,Zindel在加拿大卡尔加里大学领导的小组中继续他的研究,因为他们在腹腔巨噬细胞研究领域处于世界领先地位。由于Zindel的临床专业知识和加拿大研究人员的技术诀窍,有可能开发出一种新的成像系统,使用高级显微镜可以看到活体内部,在巨噬细胞成形并导致粘附时,将其捕获在标记物和薄膜上。这项研究成果近日发表在Science上。
巨噬细胞存在于腹腔液,它是腹膜之间的润滑剂,巨噬细胞在这种液体中被动游动,很像海洋中的浮游生物。他们的任务包括消灭病原体,同时也要尽快封闭腹腔内的损伤。它们是如何识别损伤并转移到受伤部位的,直到现在还不清楚。由于这些细胞在试管中的行为方式与它们在体内非常不同,Zindel和Candinas开发了一种新的显微镜技术,使他们能够利用腹壁最薄的部分作为观察腹膜腔的窗口,这是这些巨噬细胞的“原生栖息地”,并在它们四处移动时对其进行拍摄。
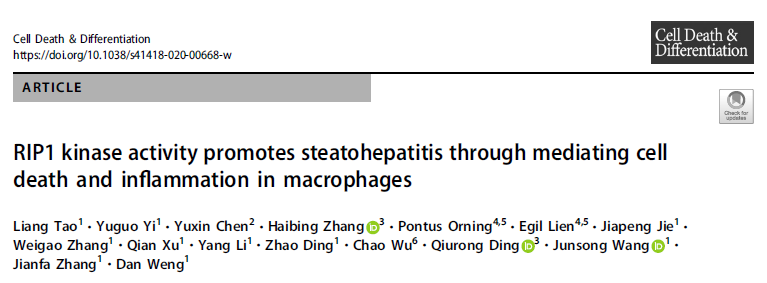
当腹腔内有损伤时,巨噬细胞在几分钟内聚集形成血块样结构。这样,它们就把伤口封起来了。研究人员发现,这背后的分子机制是基于巨噬细胞可识别各种结构的非特异性受体,这些受体在液体中移动,从而在伤口周围开始凝血。然而,当手术打开腹壁,或者植入异物造成的更大的损伤中,巨噬细胞会失去控制——血栓不会停止生长并形成长链,这些长链就是导致粘连的原因。
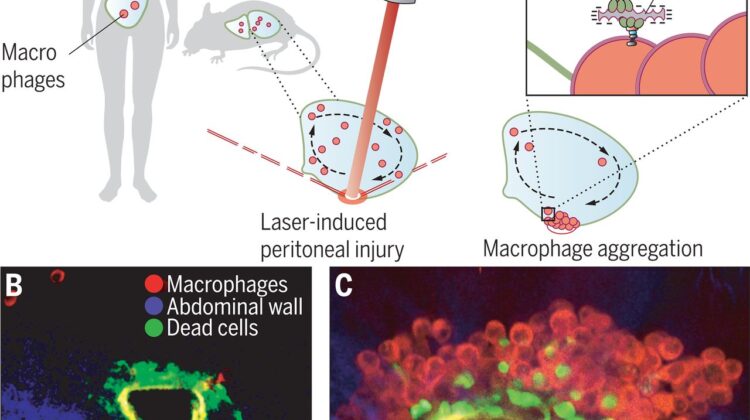
巨噬细胞将伤口封闭在体腔内
研究人员发现,当老鼠体内相应的受体被阻断时,粘连就会减少。因此,已经有人提出使用活性成分对抗粘附并已经申请专利。这一发现与许多研究领域有关,因为没有其他免疫细胞像腹腔中的巨噬细胞那样迅速被招募。类似的机制可能存在于其他脏器,如心脏或肺部,或者可能不仅在受伤中发挥作用,也可能在疾病中发挥作用,如腹部肿瘤。
总之,这项研究结果揭示了巨噬细胞的血小板样血管外液相反应。这种快速反应能在几分钟内封住腹膜渗漏,在修复局部热损伤或激光引起的腹膜损伤等小损伤方面发挥重要作用。相比之下,医源性手术,如腹部手术植入异物,反映了一种较大的损伤类型。在这种情况下,腹腔巨噬细胞可能会造成有害的疤痕,而不是恢复整合,试图修复伤口。因此,巨噬细胞聚集和清道夫受体拮抗剂对其的抑制作用具有重要的临床意义,并可能成为预防腹膜手术后瘢痕形成的治疗靶点。此外,这些发现可能延伸到其他腔脏器,包括胸膜和心包腔。
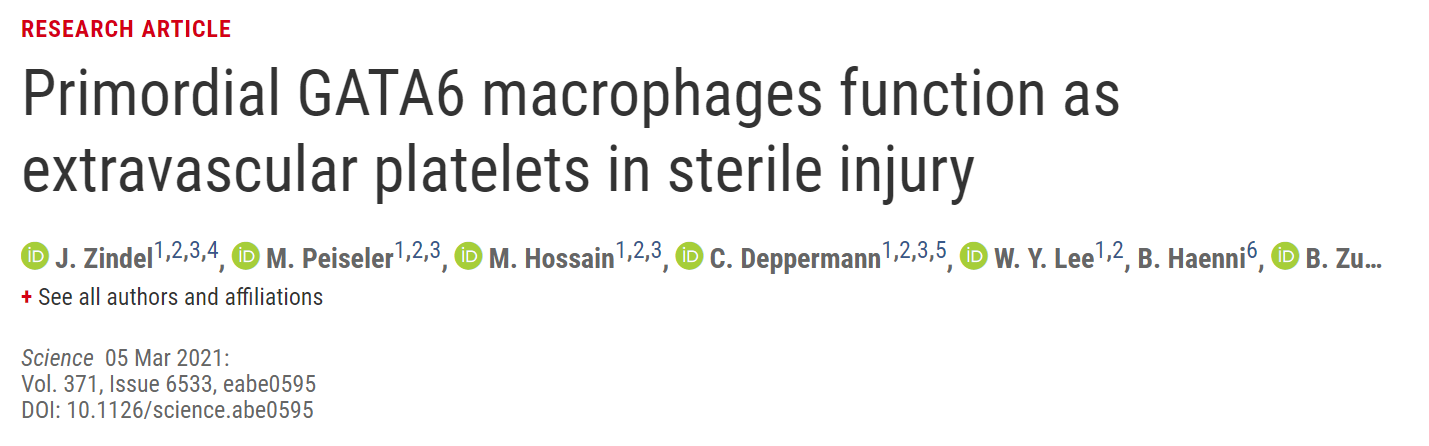
参考文献:J. Zindel, M. Peiseler, M. Hossain, C. Deppermann, W. Y. Lee, B. Haenni, B. Zuber, J. F. Deniset, B. G. J. Surewaard, D. Candinas, P. Kubes. Primordial GATA6 macrophages function as extravascular platelets in sterile injury. Science, 2021 DOI: 10.1126/science.abe0595
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#腹腔粘连#
32
#SCIE#
44
#损伤#
39
#ATA#
34