肺动脉瓣粘液瘤1例
2020-04-20 张枢书 王晶晶 医学影像学杂志
患者女11岁。活动后气促1月入院。查体:心率92次/min,呼吸20次/min,患儿发育尚可,无重要病史记载。心脏CTA检查:右心室腔内可见一结节样较均匀低密度影,CT值约20HU,病灶大小约28.7
患者女11岁。活动后气促1月入院。查体:心率92次/min,呼吸20次/min,患儿发育尚可,无重要病史记载。心脏CTA检查:右心室腔内可见一结节样较均匀低密度影,CT值约20HU,病灶大小约28.7mm×22.4mm,边缘锐利,强化不明显,病变与肺动脉瓣分界不清,右心房、右心室增大(图1,2)。
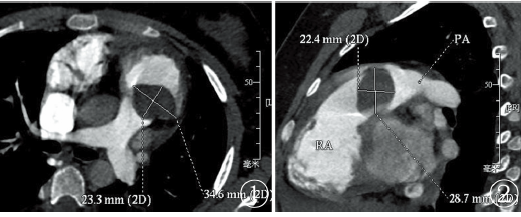
图1,2 心脏CTA肺动脉瓣可见类圆形低密度充盈缺损区,病灶向右心室腔内生长
经食管和胸超声检查:病灶位于肺动脉瓣及右室流出道(图3),大小约29.5mm×22.0mm,瘤蒂较细,长约4.8mm,瘤蒂位于右室流出道外侧壁,肿块于收缩期进入肺动脉瓣口,导致肺动脉瓣口血流受阻,三尖瓣重度返流,面积11.4 cm2,返流速度320 cm/s,PG:41mmHg。病理诊断:肺动脉瓣粘液瘤(图4)。
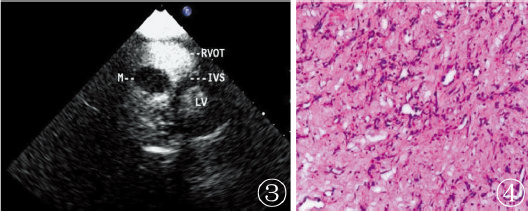 图3 心脏彩超示类圆形病灶位于肺动脉瓣及右室流出道呈低回声改变;图4 病理显示病灶表面光滑,切面灰白,小灶灰红,实性,质软,粘液样
图3 心脏彩超示类圆形病灶位于肺动脉瓣及右室流出道呈低回声改变;图4 病理显示病灶表面光滑,切面灰白,小灶灰红,实性,质软,粘液样
讨论
粘液瘤是心内最常见的良性肿瘤,可发生于心脏各个腔室,以左心房多见,约占3/4,右心房次之、右心室少见,而以发生在肺动脉瓣的粘液瘤则更为罕见。患者临床表现、心电图及胸片检查缺乏特异性,单凭肺动脉瓣区杂音易误诊为肺动脉瓣狭窄。虽然肺动脉瓣粘液瘤为良性肿瘤,但是因为瘤体阻塞肺动脉瓣,引起三尖瓣返流,右心房负荷增大,继发引起肺动脉高压,粘液瘤脱落进入肺动脉,还可引起肺动脉栓塞。
笔者认为因为肺动脉瓣粘液瘤位置的特殊性,一旦发现肺动脉瓣粘液瘤应及早手术切除,避免发生严重的肺动脉栓塞或心脏的不可逆损害。本例患者术前CTA检查诊断为血栓,是因对肺动脉瓣粘液瘤的认识不足,通常右心室血栓是由于上腔静脉血栓汇入右心房经三尖瓣进入右心室内,所以术前CTA检查将右心室内肺动脉瓣粘液瘤误认为血栓。
心脏超声检查可以动态观察粘液瘤的蒂,可见粘液瘤随心脏的收缩,规律运动,其活动范围取决于蒂的长短,而心脏内的血栓是无蒂的,以此不同之处可以鉴别粘液瘤和血栓。
综上所述,心脏超声对于心脏肿瘤的诊断仍然具有较高的价值,而CTA可以更为直观的观察瘤体的大小、形态及与周围结构的关系,通过心脏超声和心脏CTA的组合检查,可以更为准确的诊断肺动脉瓣粘液瘤,为临床尽早手术提供重要的参考依据。
原始出处:
张枢书,王晶晶.肺动脉瓣粘液瘤1例Pulmonary valve myxoma: one case report[J].医学影像学杂志,2019,29(02):272+303.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#粘液瘤#
42
#肺动脉瓣#
34
#肺动脉瓣粘液瘤#
21