JAMA Inter Med:无心衰ST段抬高型心梗:醛固酮受体拮抗剂也有获益
2018-06-02 文韬 中国循环杂志
美国一项Meta分析显示,无心衰的STEMI患者使用醛固酮受体拮抗剂也可能带来生存获益,且能改善左室射血分数。
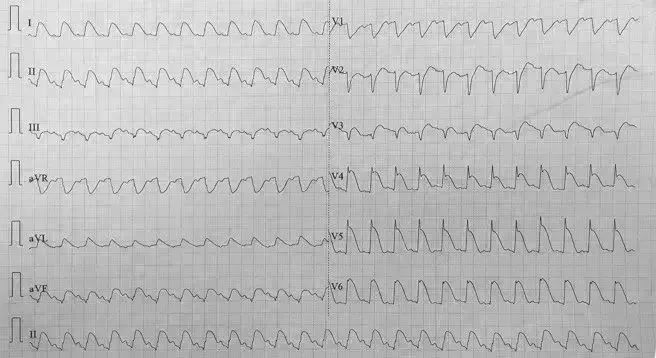
目前我国和欧美的指南建议,ST段抬高型心肌梗死(STEMI)合并LVEF≤40%的患者使用醛固酮受体拮抗剂(MRA),为I类推荐。
美国一项Meta分析显示,无心衰的STEMI患者使用醛固酮受体拮抗剂也可能带来生存获益,且能改善左室射血分数。
分析纳入10项评估STEMI不合并临床心衰或左室射血分数>40%的患者使用醛固酮受体拮抗剂治疗的随机临床试验,共4147例患者,其中醛固酮受体拮抗剂组2093例,对照组2054例。涉及的药物包括螺内酯、依普利酮和坎利酸钾等。
结果显示,对于无心衰的STEMI患者,与对照组相比,醛固酮受体拮抗剂可降低死亡风险(OR=0.62);两组心肌梗死、新发充血性心衰和室性心律失常风险相似。
与对照组相比,醛固酮受体拮抗剂可改善左室射血分数(平均差异 1.58%),轻度升高血钾水平(平均差异 0.07 mEq/L),血肌酐水平无显著变化。
原始出处:Dahal K, et al. Aldosterone Antagonist Therapy and Mortality in Patients With ST-Segment Elevation Myocardial Infarction Without Heart Failure A Systematic Review and Meta-analysis. JAMA Intern Med. JAMA Intern Med. Published online May 21, 2018
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ST段抬高型心梗#
53
#醛固酮受体拮抗剂#
52
#醛固酮#
30
#ST段抬高#
42
#拮抗剂#
37
#Med#
44
#ST段#
41
谢谢分享.学习了
81
了解了解.继续关注
73
好
69