JCEM:阿巴帕肽用于绝经后骨质疏松女性的心血管风险是安全的(ACTIVE研究)
2021-08-23 MedSci原创 MedSci原创
阿巴帕肽,英文名称为Abaloparatide,是PTH-I受体强有力的选择性激活剂,可以增加骨矿物质含量、骨密度以及骨强度,促进骨骼形成。
阿巴帕肽,英文名称为Abaloparatide,是由Radius Health公司研制的一种新型甲状旁腺激素相关肽(PTHrP),它是PTH-I受体强有力的选择性激活剂,可以增加骨矿物质含量、骨密度以及骨强度,促进骨骼形成, 已于2017年4月28日被FDA批准上市,其商品名称为Tymlos。阿巴帕肽经皮下注射,用于治疗处于骨折风险或对其它治疗药物无效的绝经后妇女的骨质疏松症,可有效降低新发椎体和非椎体骨折率。与特立帕肽相比,阿巴帕肽能够更好的降低骨折率和高钙血症发生率。ACTIVE 的3期试验就为阿巴帕肽的上市奠定了临床基础。
在这项临床试验中,在名为ACTIVE的临床3期试验中接受了为期18个月的阿巴帕肽或安慰剂治疗的绝经期骨质疏松患者转为接受为期24个月的开放标签阿仑膦酸钠治疗(ACTIVExtend)。接下来我们一起来解读一下ACTIVE的这项研究。
研究背景:阿巴帕肽是一种美国食品和药物管理局批准的甲状旁腺激素相关肽,用于治疗绝经后骨折高危女性的骨质疏松症。
研究目的:评估阿巴帕肽的心血管安全性。
方案设计:回顾心率(HR)、血压(BP)和心血管相关不良事件(AEs),包括主要不良心血管事件(MACE)和心力衰竭(HF)。
(a)ACTIVE (NCT01343004):一项3期试验,共有2463名绝经后骨质疏松女性随机服用阿巴帕肽、特立帕肽或安慰剂18个月;
(b)ACTIVExtend(NCT01657162):阿巴帕肽组和安慰剂组的参与者均接受阿仑膦酸钠治疗2年;
(c)此项目也是一项针对55名健康成年人的药理学研究
结果:阿巴帕肽和特立帕肽相对于安慰剂可暂时增加HR。第一次给药后,阿巴帕肽从治疗前到治疗后1小时的平均(标准差[SD])心率变化为每分钟7.9(8.5)次,特立帕肽为5.3(7.5)次,安慰剂为1.2(7.1)次。在随后的访问中也观察到类似的变化。

表1 ACTIVE患者就诊时心率从给药前到给药后1小时的平均变化
在健康志愿者中,在4小时内心率加快便会消失。
 图1 健康受试者单次服用阿巴帕肽与安慰剂后24小时内心率变化(90% CI);
图1 健康受试者单次服用阿巴帕肽与安慰剂后24小时内心率变化(90% CI);
BPM判定为健康受试者静息心率的预期变异值
治疗后1小时卧立位的平均收缩压和舒张压相应变化分别为-2.7 / -3.6 mmHg(阿巴帕肽)、-2.0 / -3.6 mmHg(特立帕肽)和-1.5 / -2.3 mmHg(安慰剂)。
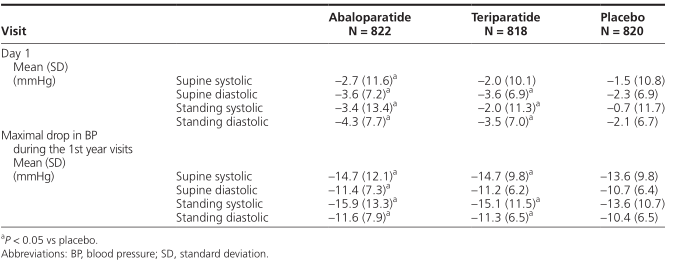
表2 给药前到给药后1小时血压变化
各组间患有严重心脏AEs的比例相似(0.9%~1.0%)。

表3 在ACTIVE中可能与心率增加相关的治疗紧急不良事件
在一项回顾性分析中,阿巴帕肽(P = 0.02 vs安慰剂)和特立帕肽(P = 0.04 vs安慰剂)首次发生MACE + HF的时间更长。

表4 在ACTIVE中MACE和MACE + HF
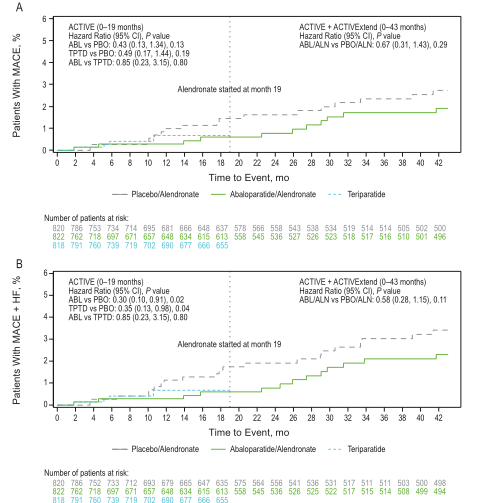
图2 ACTIVE和ACTIVExtend中MACE和MACE + HF首次发病的时间。
A) ACTIVE和ACTIVExtend 的MACE; B)ACTIVE和ACTIVExtend MACE + HF。
ABL 阿巴帕肽;ALN 阿仑膦酸钠;HF:心力衰竭;MACE:主要心血管不良事件;mo 月份;PBO安慰剂;TPTD 特立帕肽。
结论:阿巴帕肽与绝经后骨质疏松妇女的短暂心率加快和血压小幅度下降有关,但不增加严重心脏AEs、MACE或心衰的风险。
注:MACE是Major Adverse Cardiovascular Events的缩写,即主要心血管不良事件,其主要包括三个终点事件:心血管死亡、心肌梗死和卒中。
原始出处:
Cosman F, Peterson LR, Towler DA, Mitlak B, Wang Y, Cummings SR. Cardiovascular Safety of Abaloparatide in Postmenopausal Women With Osteoporosis: Analysis From the ACTIVE Phase 3 Trial. J Clin Endocrinol Metab. 2020. 105(11).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCEM#
35
#血管风险#
36
#active#
40
#JCE#
26
#阿巴帕肽#
32
#绝经#
26
#骨质#
32
#绝经后#
30
骨质疏松与甲状旁腺激素关系密切
53
学到了
73