JACC:采用双重抗血小板治疗的ACS患者或许不需停用氯吡格雷5天后才能进行冠脉搭桥术
2021-03-15 Nebula MedSci原创
采用双重抗血小板治疗的ACS患者一定要停用氯吡格雷5天后才能进行冠脉搭桥术吗?
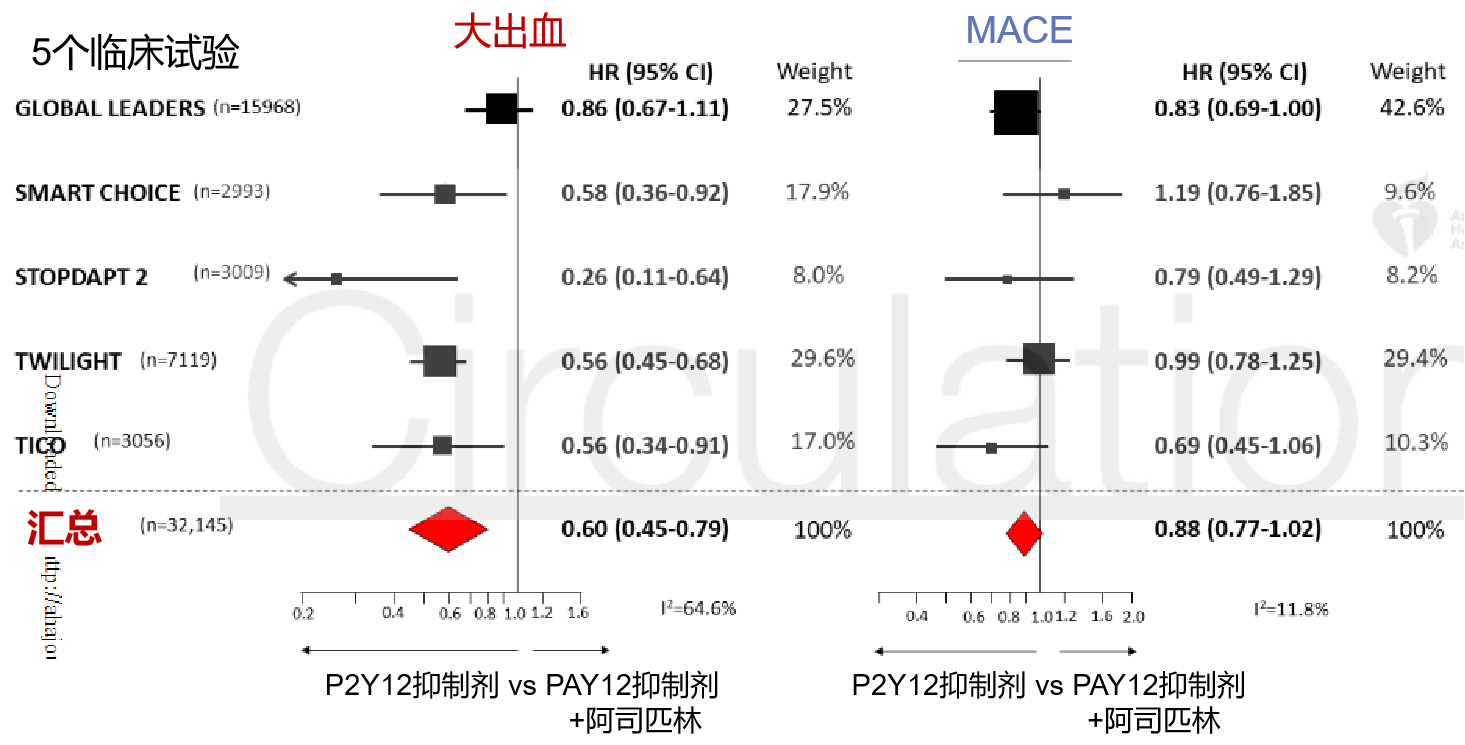
双重抗血小板治疗被推荐用于急性冠脉综合征(ACS)患者。约有10%-15%的这类患者会接受冠状动脉旁路移植术(CABG)以治疗指标性事件,目前的指南推荐在CABG前至少5天停用氯吡格雷。该等待时间具有临床和经济意义。
本研究旨在评估基于血小板反应性的策略是否不逊于CABG术后24小时出血的标准护理。
这是一项开放性非劣势试验,招募了190例有CABG指征的并服用阿司匹林和P2Y12受体抑制剂的ACS患者,分至对照组或干预组;对照组在CABG前5~7天停用P2Y12受体抑制剂,干预组在血小板反应性正常化后的下一个工作日进行CABG。
主要预后
在CABG后的第一个24小时内,干预组和对照组的胸腔引流液分别为350 ml(四分位数范围[IQR]:250~475 ml)和350 ml(255~500 ml)(P<0.001)。从决定接受CABG到手术的中位等待时间分别为112 h(IQR:66~142 h)和136 h(112~161h)(P<0.001)。
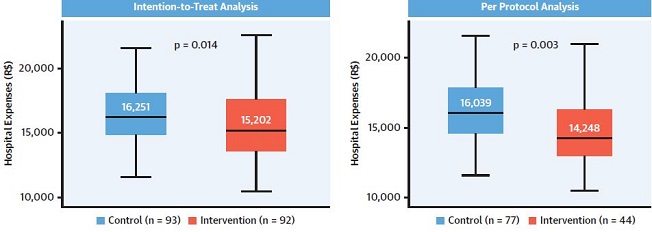
住院费用
在意向治疗分析中,干预组的中位住院费用减少了6.4%(p=0.014),在按方案分析中减少了11.2%(p=0.003)。
综上,基于血小板反应性为导向的治疗策略对ACS患者围术期出血的护理效果不逊于标准方案,而且显著缩短了等待冠脉搭桥术的时间,减少了住院费用。
原始出处:
Nakashima Carlos A K,Dallan Luis A O,Lisboa Luiz A F et al. Platelet Reactivity in Patients With Acute?Coronary Syndromes Awaiting Surgical Revascularization. J Am Coll Cardiol, 2021, 77: 1277-1286.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#冠脉搭桥术#
49
#JACC#
45
#搭桥#
51
#ACS#
34
#ACC#
35
#双重抗血小板治疗#
38
#搭桥术#
43
#冠脉搭桥#
39
#ACS患者#
48
学习学习
0