Circulation:木炭水烟可引起年轻成人急性内皮功能障碍
2019-02-23 国际循环编辑部 国际循环
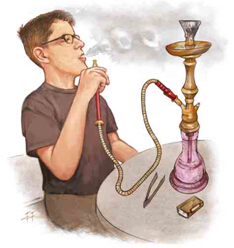
水烟被作为一种无害的香烟替代品常向年轻人推销。吸烟严重损害内皮功能,但吸入水果味水烟烟草的结果尚不清楚。传统上常用木炭加热水烟袋中的水烟烟草,水烟烟雾传递烟草毒物和尼古丁伴木炭燃烧产物:不仅富含碳的纳米粒子-氧化剂可破坏一氧化氮并损害内皮功能,而且还会产生大量血管扩张分子一氧化碳(CO)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#内皮功能障碍#
37
#功能障碍#
26
#内皮功能#
35
#水烟#
35
学习一下,谢谢分享!
71